How Can I Sleep Comfortably After Mastectomy Surgery?
Quick Answer for How to Sleep Comfortably After Mastectomy Surgery: The optimal sleeping position after mastectomy is elevated back sleeping at a 35-45 degree angle.
The optimal sleeping position after mastectomy is elevated back sleeping at a 35-45 degree angle. This position reduces pressure on surgical sites, supports lymphatic drainage, and prevents complications while allowing 6-8 hours of restorative sleep. Most patients need this positioning for 2-6 months, depending on reconstruction type.
Key positioning requirements:
-
Upper body elevation: 35-45 degrees
-
Bilateral chest protection (both sides)
-
Surgical drain accommodation if present
-
Arm support to prevent hanging or strain
Mastectomy recovery sleep presents unique challenges that require specialized positioning strategies. Understanding the proper techniques and equipment can make the difference between restless nights and restorative healing sleep.
What Makes Mastectomy Sleep Recovery Different?
Mastectomy fundamentally changes your chest architecture, creating unique sleep challenges that generic post-surgical advice can't address:
Bilateral impact: Even single mastectomy affects both sides through compensation patterns and healing requirements.
Lymphatic system disruption: When lymph nodes are removed, your body's drainage system needs gravitational assistance that only specific positioning provides.
Extended timeline: Unlike shorter recoveries, mastectomy positioning needs extend 3-6 months, requiring sustainable comfort solutions.
Reconstruction variables: Immediate reconstruction, tissue expanders, or delayed reconstruction each create different positioning requirements.
The Three Core Problems Mastectomy Sleep Positioning Must Solve
-
Surgical site protection: Preventing pressure on incisions, reconstruction sites, and healing tissue
-
Drainage optimization: Supporting both surgical drain function and natural lymphatic drainage
-
Comfort sustainability: Maintaining therapeutic positioning for full sleep cycles over months
How to Sleep After Mastectomy: Step-by-Step Positioning Guide
Step 1: Create Your Elevation Foundation
Target angle: 35-45 degrees upper body elevation Setup process:
-
Position firm wedge pillow or stacked firm pillows on bed
-
Test angle—should feel like a comfortable recliner
-
Ensure gradual incline, not sharp bend at waist
-
Add non-slip material if pillows slide
The Sleep Again Pillow System eliminates setup guesswork with pre-calibrated angles designed specifically for mastectomy recovery.
Step 2: Position Your Arms for Protection
Key principle: No part of either arm should hang unsupported
-
Support surgical side arm at natural angle using firm pillow
-
Also support non-surgical arm to prevent compensation strain
-
Ensure no pulling or stretching sensation in chest area
The Sleep Again Pillow System incorporates two side pillows for arm support during mastectomy recovery.
Step 3: Manage Surgical Drains (If Present)
-
Create secure drainage station beside bed
-
Ensure adequate tubing slack for movement
-
Use drain holders to prevent pulling
-
Position drains lower than surgical sites
Sleep Again Pillows offers surgical drain holders to help during your mastectomy recovery.
Step 4: Create Barriers to Prevent Rolling
-
Place firm pillows along surgical side
-
Position additional pillow behind back if side sleeping
-
Test barriers by gently pushing against them
The Sleep Again Pillow System incorporates two side pillows to prevent rolling while sleeping or resting during mastectomy recovery.

Optimal Sleeping Positions After Mastectomy Surgery
Position #1: Elevated Back Sleeping (Primary Position)
Best for: All mastectomy patients, especially first 6-8 weeks
Benefits:
-
Reduces swelling and fluid accumulation
-
Minimizes pressure on surgical sites
-
Easier bed entry and exit
-
Accommodates surgical drains effectively
The Sleep Again Pillow System maintains this critical 40-degree angle consistently throughout the night, unlike household pillows that compress and lose therapeutic positioning when you need support most.
Position #2: Supported Side Sleeping (Secondary)
When to try: After 2-4 weeks with surgeon approval
Side sleeping setup:
-
Firm pillow behind back prevents rolling onto surgical side
-
Support surgical side arm with pillow "nest"
-
Pillow between knees for spinal alignment
The Sleep Again Pillow System uses contoured side pillowsto provide dedicated bilateral arm support that maintains positioning throughout the night.
What Sleeping Positions to Avoid After Mastectomy
Never Sleep in These Positions:
❌ Stomach/chest sleeping
-
Direct pressure on surgical sites
-
Can displace reconstruction tissue
❌ Flat back sleeping (0 degrees)
-
Prevents lymphatic drainage
-
Increases swelling and discomfort
❌ Surgical side sleeping
-
Direct pressure on healing tissue
-
Risk of implant displacement
Timeline: How Long Do I Need Special Positioning?
Simple Mastectomy:
-
Weeks 1-4: Strict elevation (40-45 degrees)
-
Weeks 5-8: Gradual expansion (35-40 degrees)
-
Weeks 9-12: Transition to normal positions
Mastectomy with Immediate Reconstruction:
-
Weeks 1-6: Strict elevation (40-45 degrees)
-
Weeks 7-12: Gradual expansion (35-40 degrees)
-
Months 4-6: Careful transition to normal positions
Bilateral Mastectomy:
-
Weeks 1-6: Strict bilateral protection
-
Weeks 7-16: Gradual expansion with continued elevation
-
Months 5-8: Transition with ongoing precautions

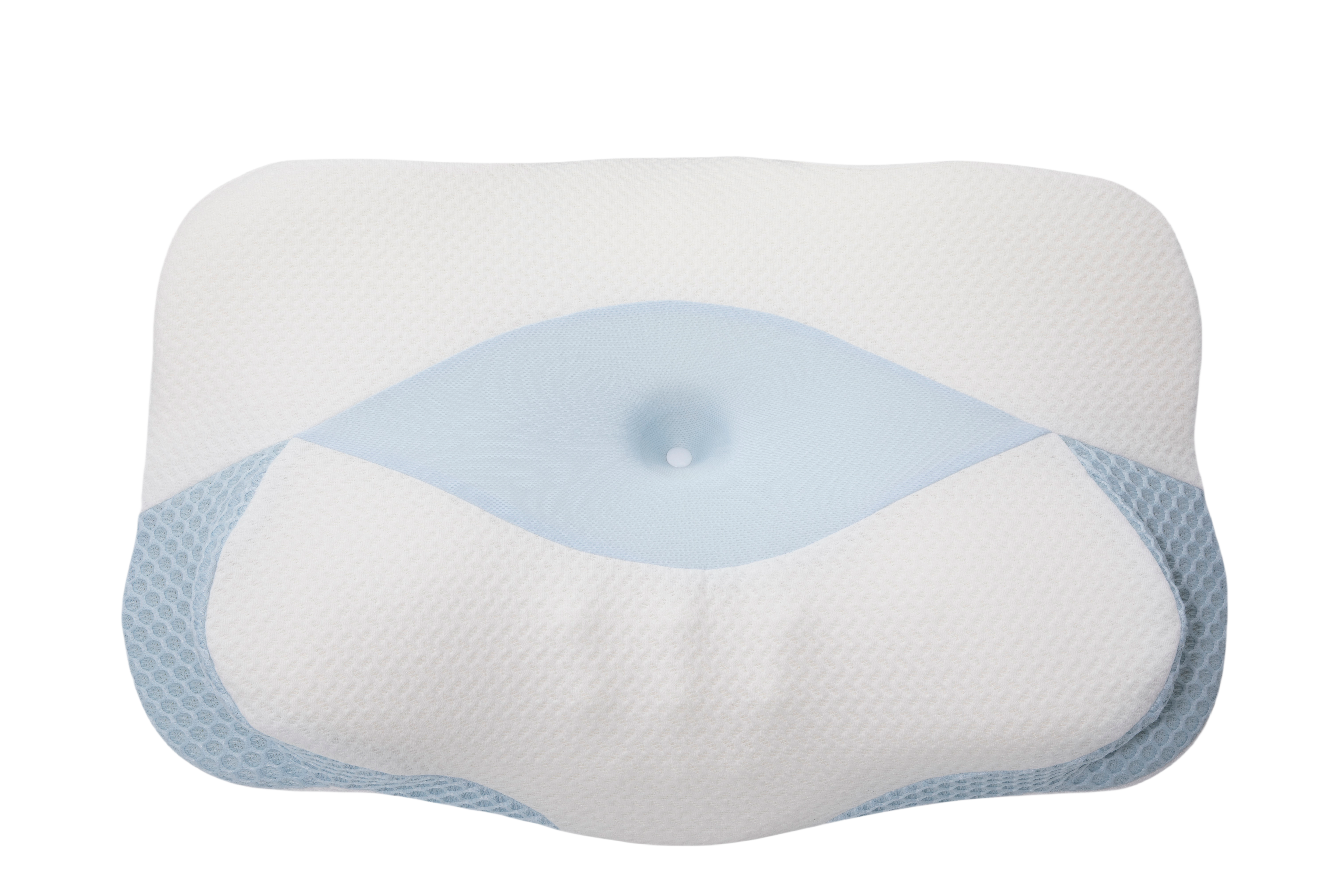
The Sleep Again System: Professional-Grade Mastectomy Recovery Solution
The Sleep Again Pillow System represents the only positioning system specifically engineered for mastectomy recovery's complex requirements.
Complete Sleep Again Pillow System Includes:
-
Upper Body Wedge (perfect 40-degree angle for mastectomy recovery)
-
Two Contoured Side Pillows (bilateral chest protection)
-
Leg Support Wedge (comprehensive drainage support)
-
Head Pillow (extended elevation comfort)
-
Medical-grade washable covers
Why the Sleep Again Pillow System Excels for Mastectomy Recovery
Mastectomy-specific engineering:
-
Precise 40-degree elevation optimized for lymphatic drainage
-
Bilateral protection design prevents rolling onto either side
-
Drain-compatible spacing accommodates medical tubing
-
Extended recovery construction maintains shape for months
Professional advantages over DIY solutions:
-
3-minute setup vs 15-20 minutes with household pillows
-
Maintains therapeutic positioning all night
-
HSA/FSA eligible as durable medical equipment
-
Designed for 3-6 month recovery periods
The Sleep Again Pillow System and its integrated design eliminate the trial-and-error period typical with individual pillow purchases, providing immediate therapeutic positioning from night one.
Cost Comparison: DIY vs Sleep Again System
DIY Pillow Approach:
-
Cost: $200-400 across multiple purchases
-
Setup: 15-20 minutes nightly
-
Maintenance: 2-4 wake-ups for readjustment
Sleep Again Pillows:
-
Complete system: $299 (HSA/FSA eligible)
-
Setup: 3-5 minutes once familiar
-
Maintenance: Maintains position throughout sleep
The Sleep Again Pillow System and its professional construction provide consistent therapeutic angles that household pillows simply cannot match, making it a cost-effective investment in recovery success.
SHOP THE BEST PILLOW SYSTEM FOR MASTECTOMY RECOVERY
Common Mastectomy Sleep Problems and Solutions
"I keep sliding down my elevation setup."
Solution: Use a firm wedge pillow with a non-slip base.
Sleep Again Pillow System advantage: Non-slip wedge design prevents sliding throughout the night
"My surgical drains make positioning impossible."
Solution: Create dedicated drain stations with proper tubing slack
Sleep Again Pillow System advantage: System spacing accommodates drain tubing without kinking
"I can't find comfortable arm positions."
Solution: Use firm pillows to create "nests" for both arms
Sleep Again Pillow System advantage: Contoured side pillows provide dedicated bilateral arm support
"My partner can't sleep with all the pillows."
Solution: Use integrated positioning system designed for shared beds
Sleep Again Pillow System advantage: Modular design uses less space than DIY setups while providing superior support
Managing Mastectomy Sleep with Reconstruction
Immediate Reconstruction Considerations
Implant-based reconstruction:
-
Requires longer elevation periods (6-8 weeks minimum)
-
Positioning must prevent implant displacement
Flap reconstruction:
-
Creates compound positioning requirements
-
May need protection of tissue source sites
Tissue Expander Management
-
Each expansion may change positioning needs
-
Requires flexible system adapting to size changes
-
The Sleep Again Pillows accommodate these evolving requirements without requiring new equipment purchases
The Sleep Again System Pillow System’s modular components adapt to reconstruction changes, providing consistent support throughout the entire recovery journey.
Frequently Asked Questions
Q: What is the best sleeping position immediately after mastectomy surgery?
A: Elevated back sleeping at 40-45 degrees is optimal. This reduces swelling, supports drainage, and protects surgical sites.
Q: How long do I need to sleep elevated after a mastectomy?
A: 6-12 weeks, depending on surgery type. A simple mastectomy may require 6-8 weeks, while reconstruction often requires 12+ weeks.
Q: Can I sleep on my side after mastectomy surgery?
A: Side sleeping on your non-surgical side may be possible after 3-4 weeks with surgeon approval and proper support.
Q: What pillows work best for mastectomy recovery sleep?
A: Professional systems like the Sleep Again Pillow System provides consistent therapeutic positioning that household pillows cannot match, with mastectomy-specific engineering for optimal recovery support.
Q: How do I sleep with surgical drains after mastectomy?
A: Create secure drainage stations beside your bed with adequate tubing slack and proper drain positioning.
Q: Should I buy special pillows for mastectomy recovery?
A: Yes, professional positioning equipment like the Sleep Again Pillow System provides immediate benefits and continues improving sleep quality long after recovery.
When to Contact Your Healthcare Team
Call Your Surgeon Immediately For:
-
Signs of infection (redness, warmth, unusual discharge)
-
Severe pain unresponsive to medication
-
Problems with surgical drains
-
Sudden swelling increase
-
Difficulty breathing
-
Fever over 101°F
Schedule Follow-up Discussions For:
-
Sleep problems worsening after first week
-
Persistent numbness or unusual sensations
-
Questions about position advancement
-
Reconstruction healing concerns
Your Mastectomy Sleep Recovery Success Plan
Mastectomy sleep recovery success depends on understanding that positioning is medical intervention, not comfort preference. Your strategy should focus on:
Therapeutic elevation supporting lymphatic drainage and surgical healing Comprehensive protection accommodating bilateral chest surgery effects Professional equipment that maintains consistent positioning over months
The Sleep Again Pillow System addresses these interconnected requirements through mastectomy-specific engineering rather than adapted general solutions. This eliminates trial-and-error periods while providing consistency supporting both physical healing and psychological adjustment.
The Sleep Again Pillow System's construction ensures therapeutic positioning remains consistent throughout months of recovery, making it an investment in both immediate comfort and long-term healing success.
Most importantly, recognize that mastectomy recovery positioning extends for months, not weeks. The positioning strategies you establish often continue providing benefits indefinitely, making the Sleep Again System an investment in lifelong sleep quality rather than temporary medical accommodation.
Medical Disclaimer
This information is provided for educational purposes only and should not replace professional medical advice. Every mastectomy procedure and recovery process is unique, and sleeping position recommendations may vary significantly based on your specific surgical approach, reconstruction type, lymph node involvement, radiation therapy plans, individual health conditions, and post-operative circumstances.
Always follow your surgeon's specific post-operative instructions regarding sleep positioning, activity restrictions, and recovery protocols. These medical guidelines take precedence over any general positioning advice provided here.
Contact your healthcare provider immediately if you experience concerning symptoms such as signs of infection, severe pain, problems with surgical drains, sudden swelling, difficulty breathing, fever, or any symptoms that worsen during recovery.
The mention of specific products or sleeping strategies is for informational purposes only and does not constitute medical endorsement. Trust your healthcare provider's guidance above any general sleep advice, and discuss positioning concerns with your medical team.
Individual healing timelines vary significantly based on factors including age, overall health, surgical technique, reconstruction type, and adherence to post-operative care instructions.