Introduction: Understanding the Mastectomy Journey
A mastectomy represents a significant chapter in anyone's breast cancer journey. Whether performed as a treatment for existing breast cancer or as a preventive measure for those at high risk, this surgical procedure removes breast tissue from one breast (unilateral mastectomy) or both breasts (bilateral mastectomy).
Breast cancer remains the most common cancer among women in the United States, with approximately one in eight women (13%) developing invasive breast cancer during their lifetime, according to BreastCancer.org. Early detection through regular screening is essential, as the disease often presents with minimal or no symptoms initially.
This comprehensive guide provides essential information on mastectomy recovery—from pre-surgery preparation to long-term healing, with practical advice to support your journey.
Types of Mastectomy Procedures
Different mastectomy procedures require different recovery approaches:
-
Total (Simple) Mastectomy: Removes the entire breast, including the nipple and areola.
-
Modified Radical Mastectomy: Removes the breast and some lymph nodes under the arm.
-
Skin-Sparing Mastectomy: Preserves most skin over the breast while removing breast tissue.
-
Nipple-Sparing Mastectomy: Preserves the skin, nipple, and areola while removing breast tissue.
-
Preventive (Prophylactic) Mastectomy: Performed on those with high risk of developing breast cancer.
-
Double (Bilateral) Mastectomy: Removal of both breasts.
Understanding your specific procedure will help you better prepare for recovery.
Pre-Surgery Preparation
Your journey begins before surgery day. Taking time now to prepare your body, home, and mind will make a world of difference in your recovery. Think of this preparation as an act of self-care—you're giving your future self the gift of a smoother healing experience.
Medical Preparation
-
Attend all preoperative appointments
-
Discuss medications with your healthcare team
-
Understand your specific procedure and ask questions
Practical Preparation
-
Set up a recovery area on your home's main floor if possible
-
Stock up on nutritious, easy-to-prepare foods
-
Fill pain medication prescriptions in advance
-
Arrange for help with transportation and household tasks
Clothing and Personal Items
-
Select front-closing, loose-fitting shirts and pajamas
-
Choose comfortable pants with elastic waistbands
-
Prepare a hospital bag with essential personal items
-
Consider a mastectomy pillow for recovery comfort
Hospital Stay: What to Expect
The hospital phase may be brief, but it's the beginning of your healing journey. This time is all about basic recovery and learning the essentials of self-care that you'll continue at home. Trust your medical team, ask questions, and remember: every hour brings you closer to healing and home.
Length of Stay
-
Mastectomy without reconstruction: Typically 1-2 days
-
Mastectomy with immediate reconstruction: Usually 2-3 days, sometimes longer
Immediate Post-Surgery Recovery
-
Pain management is a priority
-
Nurses will monitor your surgical site and drains
-
You'll be encouraged to walk within 24 hours
-
You'll receive education about drain care and wound management
Before Discharge
-
Written instructions will be provided
-
You'll receive prescriptions for pain medication
-
Follow-up appointments will be scheduled
-
Drain care instructions will be reviewed
Managing Surgical Drains
While drains might seem intimidating at first, they're actually your allies in healing. These small devices help your body recover by removing fluid that could otherwise slow the healing process. With a little knowledge and practice, drain management will become a simple part of your daily routine—a tangible way you're participating in your own healing.
Purpose of Drains
-
Remove accumulated blood and lymphatic fluid
-
Prevent fluid buildup that could delay healing
-
Reduce swelling and discomfort
-
Decrease infection risk
Drain Care Basics
-
Wash hands before handling drains
-
Empty drains every 8-12 hours or when half-full
-
Record the amount, date, and time of drainage
-
Compress the bulb completely when resealing
-
Keep the area clean and dry
Managing Drain Discomfort
-
Use a mastectomy drain belt or specialized garment
-
Pin drains to clothing with safety pins
-
Avoid pulling or tugging on drain tubes
-
Use the Sleep Again Pillow System to position drains comfortably during rest
Drain Removal
-
Typically done at a follow-up appointment when output is minimal
-
The procedure is quick with momentary discomfort
-
Keep the site clean and covered for 24-48 hours after removal
Physical Recovery Timeline
Your body has amazing healing capabilities, working day and night to recover from surgery. Understanding what to expect week by week helps you recognize progress that might otherwise go unnoticed. Remember that healing isn't linear—some days will be better than others—but the overall trajectory is toward healing and renewed strength.
Week 1: Immediate Post-Surgery
-
Significant fatigue from surgery and anesthesia
-
Pain and discomfort at the surgical site
-
Limited arm mobility on the affected side(s)
-
Short, slow walks around the house
-
Assistance needed for many daily activities
Weeks 2-3: Early Recovery
-
Gradual decrease in pain and discomfort
-
Possible removal of some or all drains
-
Longer, more frequent walks
-
Increased independence in daily activities
Weeks 4-6: Intermediate Recovery
-
Continued improvement in comfort and healing
-
All drains typically removed by this point
-
Many patients can resume driving (with physician approval)
-
Possible return to work for non-physical jobs
Weeks 6-12: Advanced Recovery
-
More normal daily activities
-
Beginning to increase exercise intensity gradually
-
Return to work for most patients
-
Improved arm range of motion
3-6 Months: Long-Term Recovery
-
Continued softening and fading of scars
-
Return to most previous activities
-
Lifting restrictions often completely lifted by 3 months
Physical Therapy and Exercise
Movement is medicine after mastectomy. The right exercises at the right time help prevent complications and rebuild strength and mobility. Start gently, progress patiently, and celebrate each small improvement. Your body is learning a new normal, and these mindful movements are guiding that process.
Early Recovery Exercises (First 1-2 Weeks)
-
Deep breathing exercises
-
Hand and wrist exercises
-
Shoulder pumps
-
Elbow flexion and extension
Intermediate Exercises (Weeks 2-4)
-
Pendulum exercises
-
Wall slides
-
Arm slides on table
-
Shoulder blade squeezes
Advanced Recovery Exercises (Weeks 4-8)
-
Standing wall climbs (front and side)
-
Stick or wand exercises
-
Light resistance band exercises (with surgeon's approval)
Working with Physical Therapy Professionals
-
Consider therapists with experience in breast cancer rehabilitation
-
Physical therapy can provide personalized exercise programming
-
Manual therapy techniques may improve mobility and reduce scar tissue
Pain Management and Comfort
Pain is not just something to endure—it's something to manage actively and intelligently. Effective pain control supports your body's healing processes and improves your quality of life during recovery. You deserve to be comfortable, and with the right approaches, discomfort can be minimized as your body heals.
Types of Post-Mastectomy Pain
-
Incisional pain at the surgical site
-
Muscle pain from positioning or tension
-
Nerve pain (burning, shooting, or tingling sensations)
-
Referred pain in the shoulder, back, or neck
Medication Approaches
-
Follow prescribed pain medication schedules
-
Transition to over-the-counter options when appropriate
-
Consider non-opioid options as recovery progresses
Non-Medication Pain Management
-
Cold therapy for the first week
-
Warm therapy after initial healing (with doctor's approval)
-
Proper positioning with the Sleep Again Pillow System
-
Gentle movement to prevent stiffness
Optimizing Sleep During Recovery
Sleep is when your body does its deepest healing work. Creating the perfect sleep environment might be the single most important gift you can give yourself during recovery. With the right support and positioning from the Sleep Again Pillow System, you can transform restless nights into restorative sleep that actively accelerates your healing process.
Sleep Challenges After Mastectomy
-
Discomfort from surgical sites
-
Limited sleeping positions due to pain
-
Surgical drains that may pull or become tangled
-
Disrupted sleep patterns from hospital stays
Creating Optimal Sleeping Conditions
Sleep Position Strategies
-
Elevated position: Most surgeons recommend sleeping with your upper body elevated at a 30-45 degree angle
-
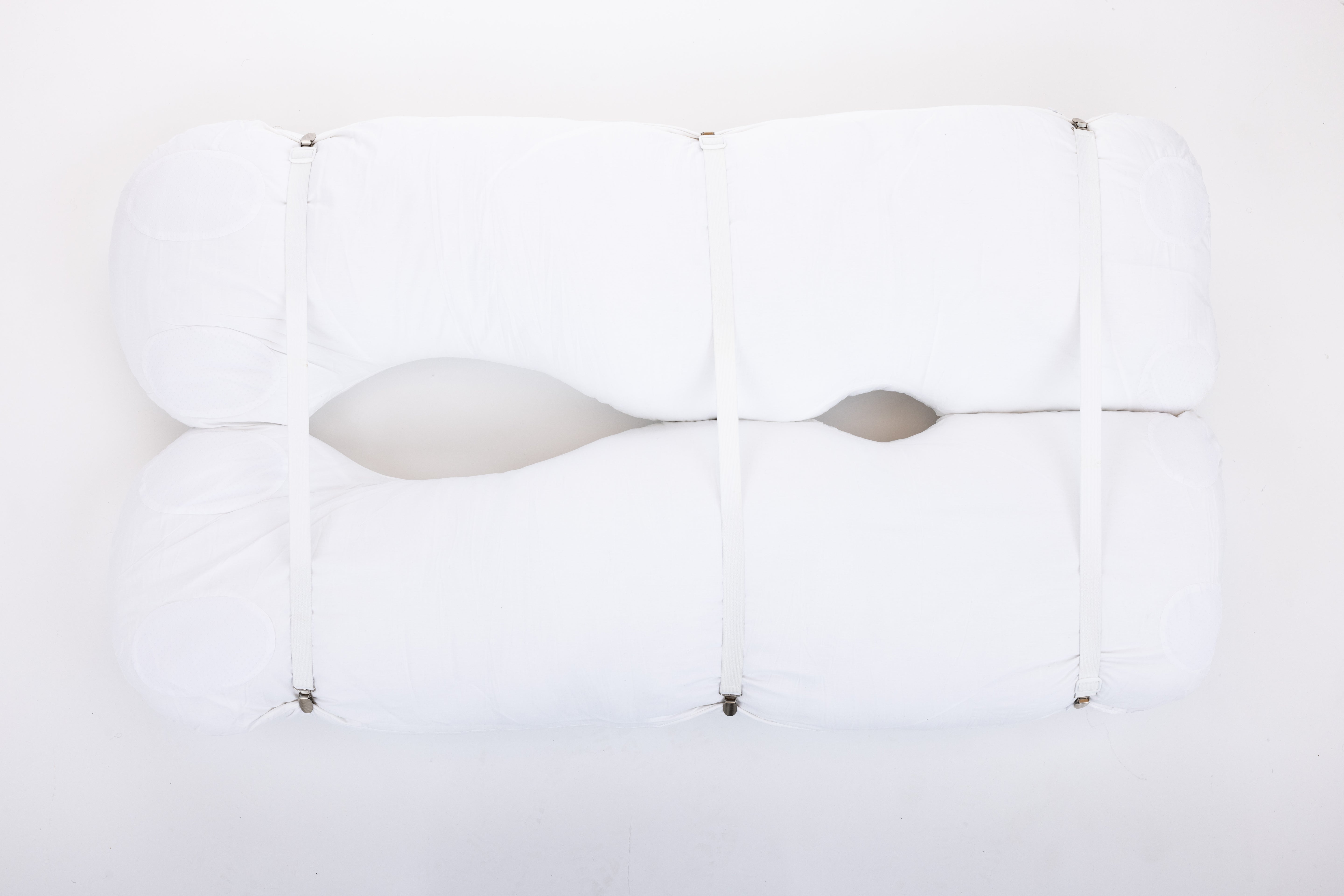
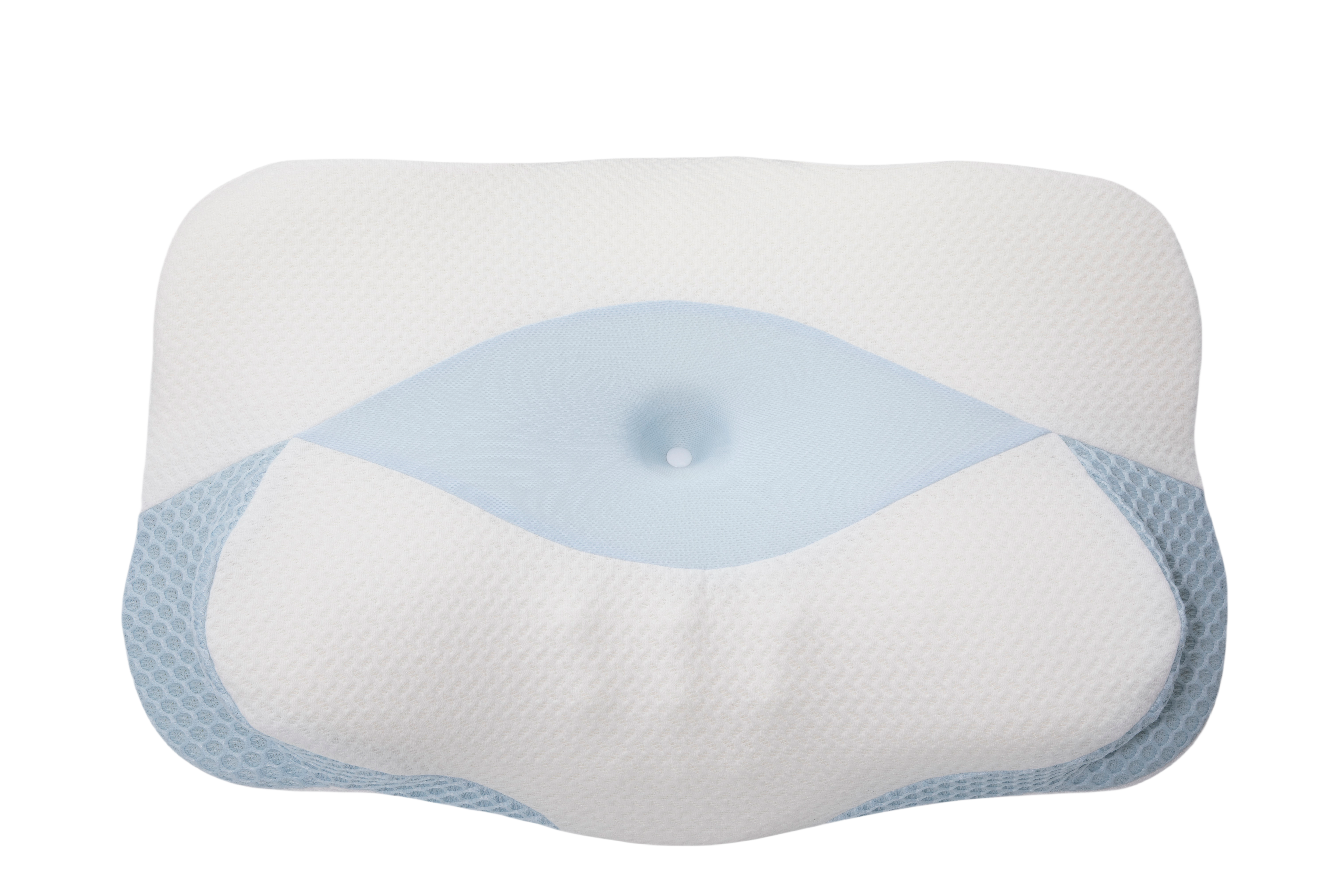
The Sleep Again Pillow System: Specifically designed for mastectomy recovery with:
-
Two wedges that provide stable elevation
-
Two full-size body pillows that prevent rolling onto surgical sites
-
A neck pillow for proper alignment
-
Adjustable components that can be customized as recovery progresses
-
A protective "cocoon" feeling that promotes both physical comfort and emotional security
Managing Pain for Better Sleep
-
Time pain medication appropriately before bedtime
-
Empty drains before sleeping to prevent middle-of-night filling
-
Secure drains properly to prevent pulling during sleep
-
Use the Sleep Again body pillows to maintain comfortable positioning all night
Nighttime Comfort Tips
-
Wear soft, non-restrictive sleepwear that opens in front
-
Have water and medications within reach
-
Use extra pillows from the Sleep Again system for repositioning if needed
Transitioning to Long-term Healthy Sleep
-
Gradually adjust sleeping position as recovery progresses
-
The Sleep Again Pillow System can be reconfigured as needs change
-
Components continue to provide value long after recovery for general sleep comfort

Wound and Scar Care
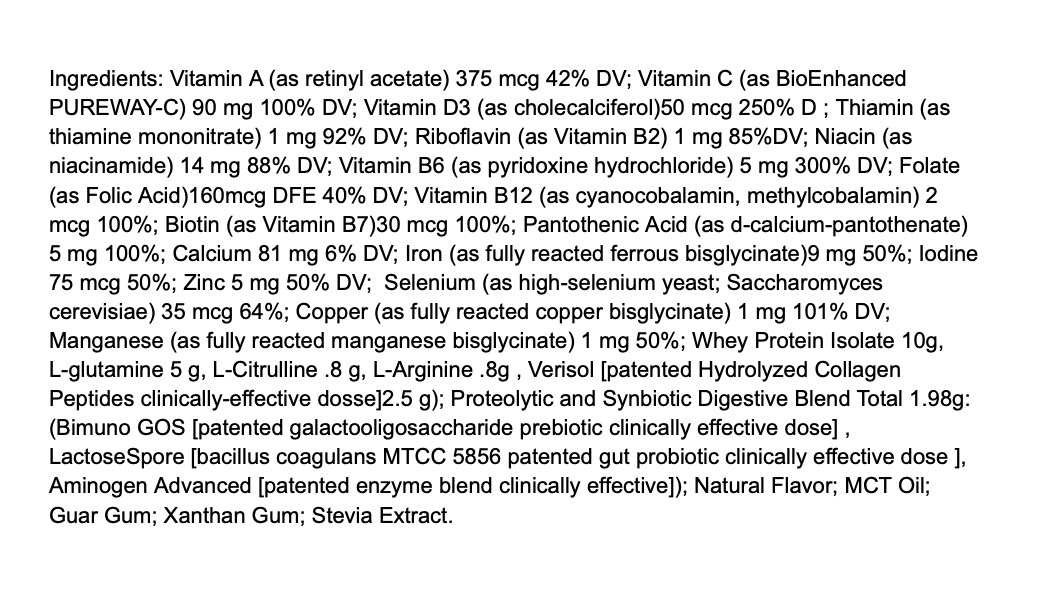
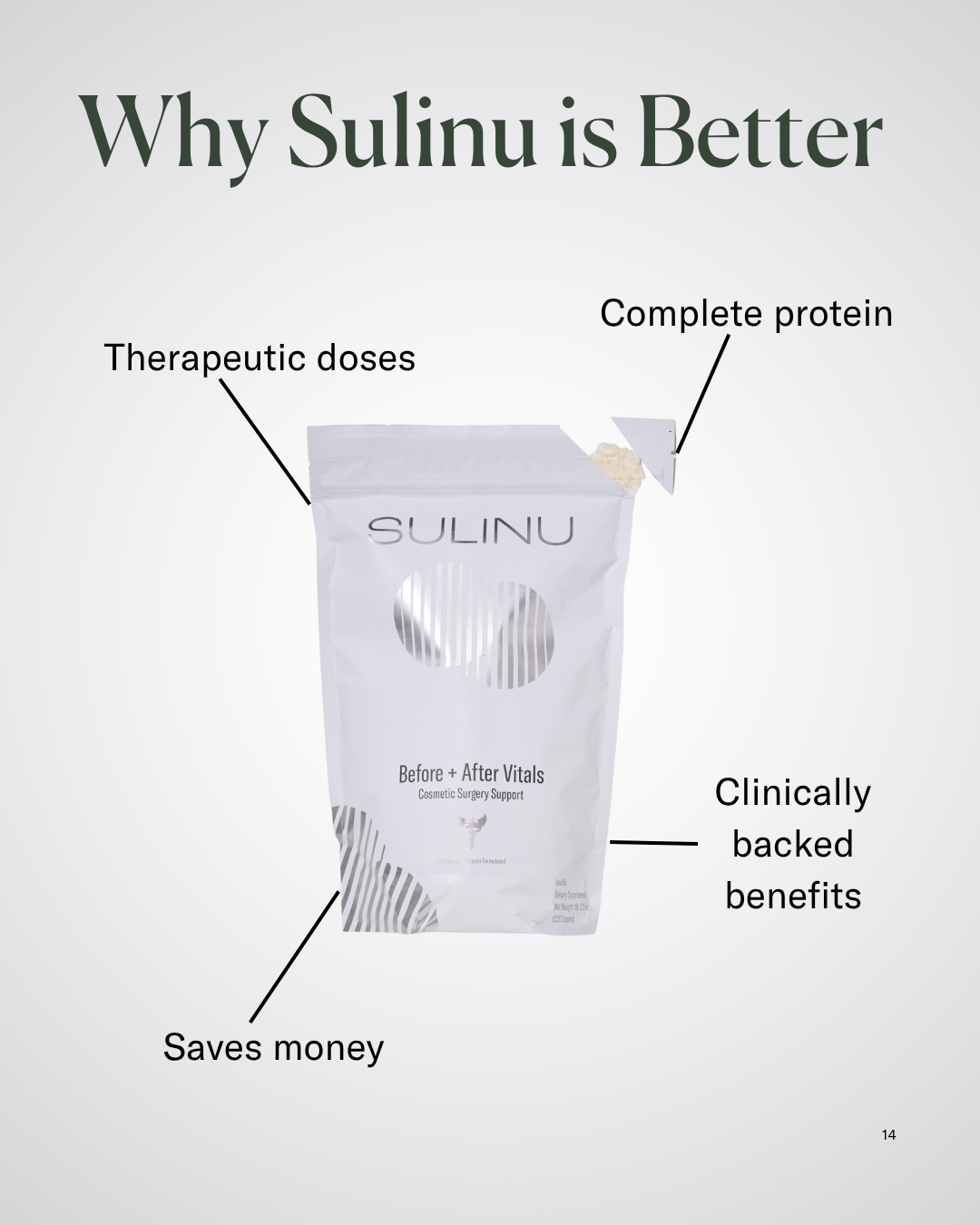
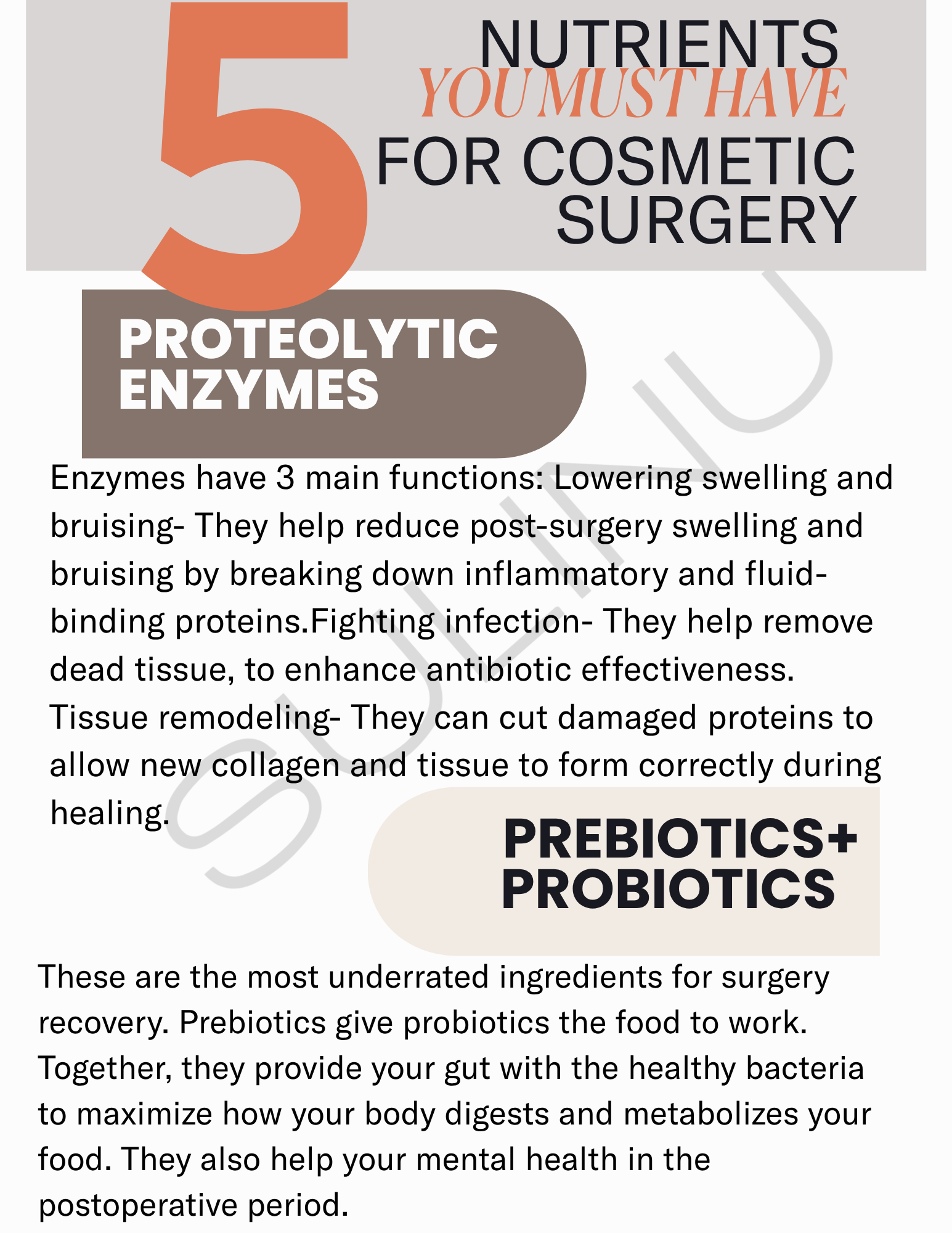
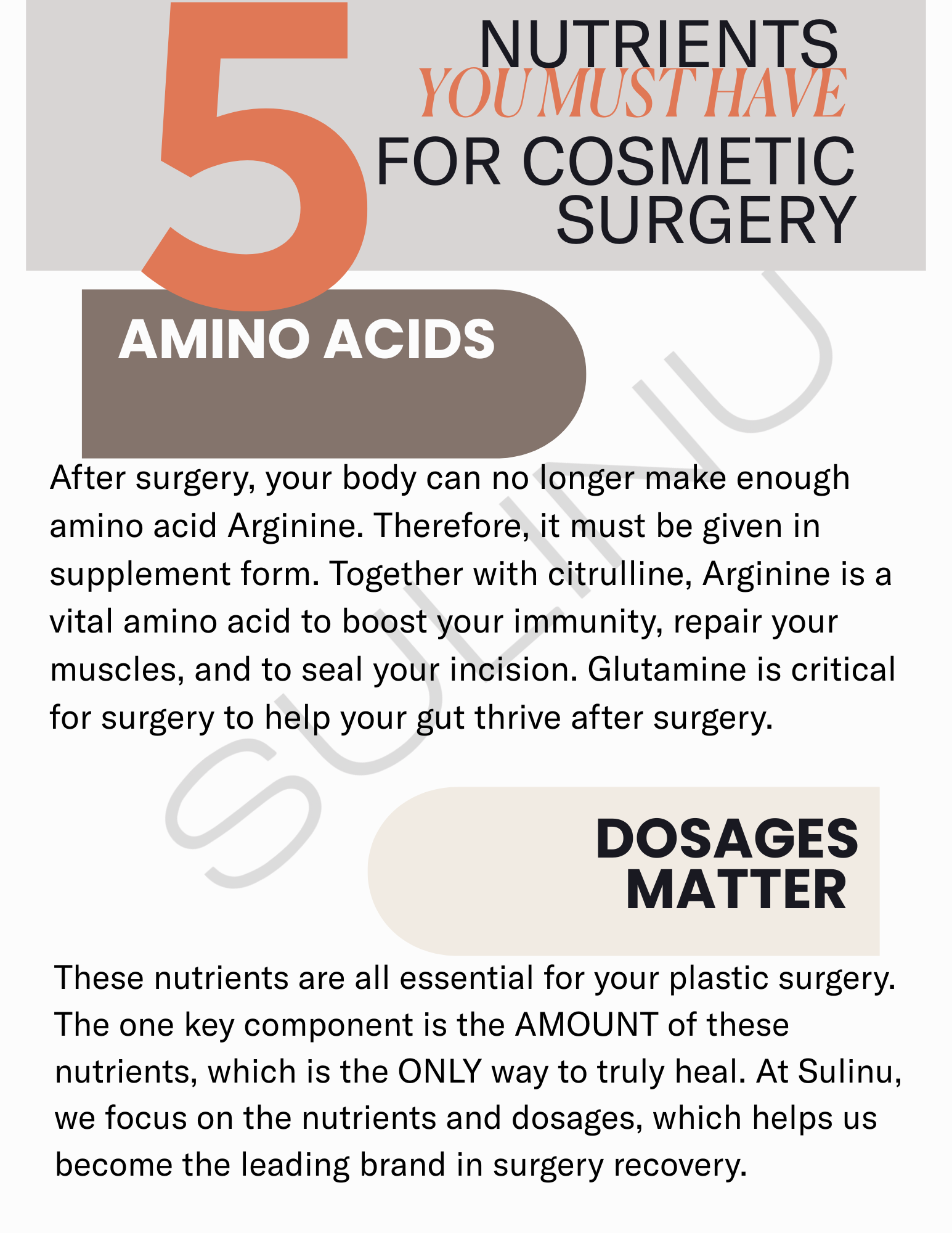
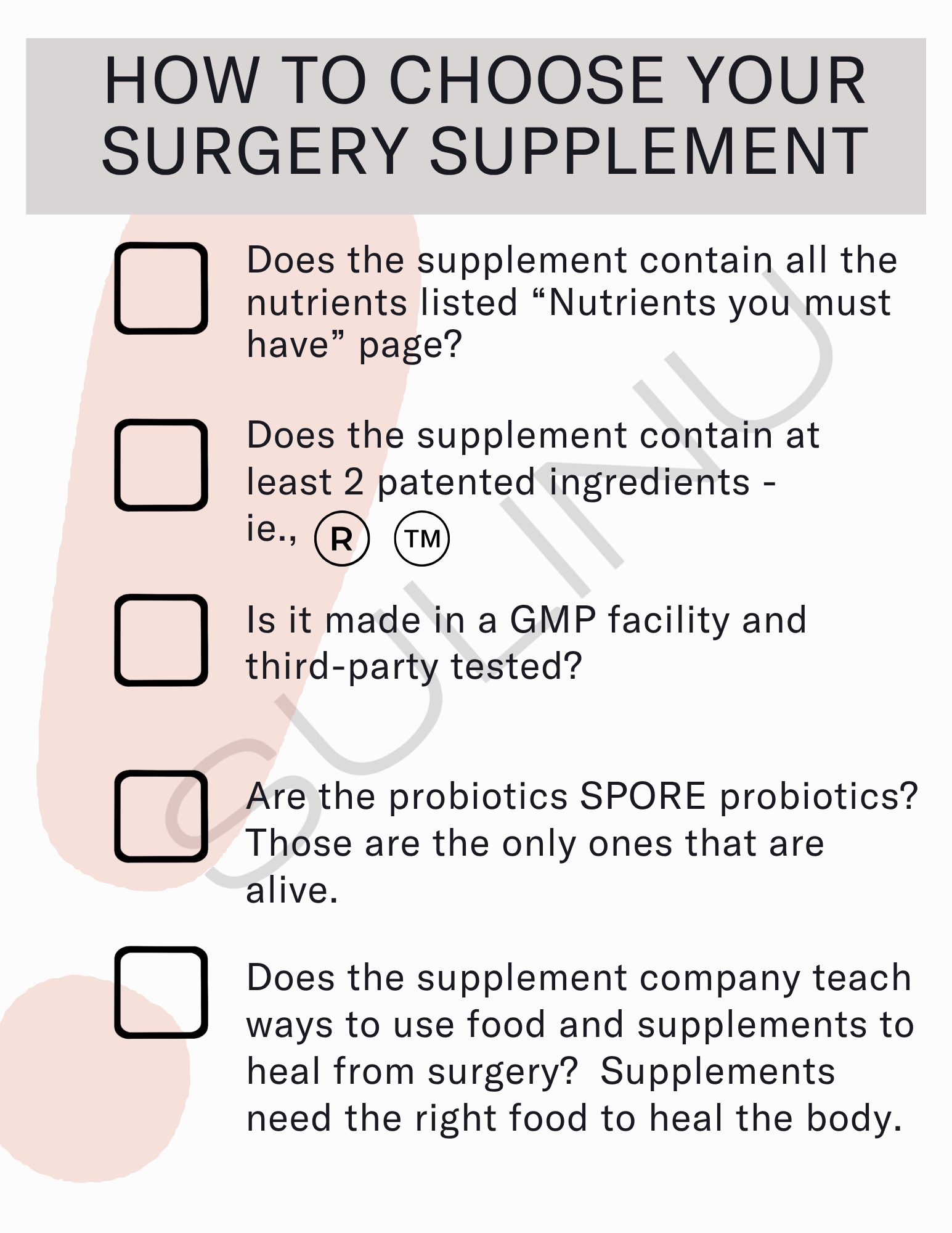
To help support your healing journey, the world's first and only wound healing supplements, Before + After Vitals, is specifically designed by a clinical dietitian for accelerated recovery, a perfect scar, and a beautiful body.
This 8-in-1 NutriSurgical vitamin powder gives you everything you need in one scoop. Formulated with bioenhanced Vitamin C, patented proteolytic enzymes, hydrolyzed collagen, and biome synbiotics, Before + After Vitals is the best pre and post-surgery recovery supplement on the market today.
Combine Before + After Vitals and the Sleep Again Pillow System for the ultimate healing duo during your mastectomy recovery.
Understanding the Healing Process
Each day of gentle attention to your healing skin helps write the next chapter—one where these marks of survival become less prominent while remaining a testament to your strength.
-
Initial inflammatory phase (Days 1-5): Swelling and redness
-
Proliferative phase (Days 5-21): New tissue formation
-
Maturation phase (21 days to 2 years): Scar remodeling
Immediate Post-Surgery Wound Care
-
Follow your surgeon's instructions for dressing changes
-
Keep the area clean and dry
-
Watch for signs of infection (increased redness, warmth, drainage)
Long-term Scar Management
-
Begin scar massage only after the incision is fully healed (typically 3-4 weeks)
-
Consider silicone-based products after complete closure
-
Protect scars from sun exposure for at least 12 months
Lymphedema Awareness and Prevention
Knowledge is power when it comes to lymphedema. Being aware of this potential side effect empowers you to take simple preventive steps and recognize early warning signs. With proactive care, many women successfully manage or avoid lymphedema entirely, allowing you to focus on moving forward with confidence.
Understanding Lymphedema Risk
-
More common when multiple lymph nodes are removed
-
Can develop shortly after surgery or years later
-
Affects the arm, hand, breast, or trunk on the surgery side
Prevention Strategies
-
Keep the affected arm clean and protected
-
Avoid blood draws or blood pressure on the affected arm when possible
-
Exercise regularly as prescribed by your healthcare team
-
Maintain a healthy weight
Early Detection
-
Learn to recognize early signs (swelling, heaviness, tightness)
-
Regularly compare measurements of both arms
-
Report symptoms promptly to your healthcare provider
Emotional and Psychological Recovery
Your emotional healing deserves as much attention as your physical recovery. The feelings that arise—from grief to gratitude, fear to freedom—are all valid parts of your journey. By acknowledging and expressing these emotions, you create space for profound healing and growth that often reaches far beyond physical recovery.
Common Emotional Responses
-
Shock and grief over body changes
-
Anxiety about healing and the future
-
Identity shifts and redefinition
-
Concerns about intimacy and relationships
Coping Strategies
-
Practice self-care with adequate rest and nutrition
-
Express feelings through journaling or creative outlets
-
Consider joining a support group
-
Work with a therapist or counselor if needed
Body Image and Identity
-
Give yourself permission to feel all emotions
-
Take time to gradually adjust to physical changes
-
Focus on what your body can do rather than only how it looks
-
Practice self-compassion and positive self-talk
Practical Considerations for Daily Life
Recovery happens in the midst of everyday life. Small adjustments to your environment and routines can make a world of difference in your comfort and independence. These practical strategies help bridge the gap between where you are now and where you want to be, making each day a little easier as you heal.
Home Setup and Modifications
-
Place commonly used items at waist to shoulder height
-
Prepare a comfortable recovery space with essentials nearby
-
Consider the Sleep Again Pillow System for comfortable positioning during daytime rest
Managing Daily Activities
-
Use front-closing garments to avoid raising arms overhead
-
Accept help with household tasks and meal preparation
-
Take a gradual approach to resuming normal activities
Child and Pet Care
-
Arrange childcare help, especially for the first 1-2 weeks
-
Modify how you interact with children to avoid lifting
-
Consider temporary assistance with pet care, especially for energetic pets
Nutrition for Optimal Healing
Food becomes medicine during recovery. What you eat directly impacts how quickly and completely you heal. Nourishing your body with healing foods is a powerful way to participate in your recovery—providing your body the building blocks it needs to repair tissue, fight infection, and regain energy.
Key Nutrients for Recovery
-
Protein: Essential for tissue repair (lean meats, fish, eggs, legumes)
-
Vitamin C: Supports collagen formation (citrus, berries, peppers)
-
Zinc: Important for cell growth (seafood, meat, beans)
-
Adequate hydration: Supports all healing processes
Practical Meal Planning
-
Prepare and freeze portions before surgery
-
Stock up on nutritious, easy-to-prepare foods
-
Consider meal delivery services temporarily
-
Keep healthy snacks easily accessible
Returning to Work and Normal Activities
Rejoining your regular life is a significant milestone in recovery. This transition happens gradually, with each resumed activity marking progress on your healing journey. Balancing your desire to return to normalcy with respect for your body's ongoing recovery is an art—one that teaches patience and self-compassion.
Timeline Considerations
-
Office/desk jobs: Often possible after 2-4 weeks
-
Physically demanding jobs: May require 6-8 weeks or longer
-
Driving: Usually resume after 1-3 weeks when no longer taking narcotic pain medication
Workplace Accommodations
-
Consider a gradual return schedule
-
Discuss necessary physical modifications
-
Allow time for follow-up appointments
Resuming Daily Activities
-
Light housework: Gradually after 1-2 weeks
-
Driving: When you can turn and react quickly (1-3 weeks)
-
Exercise: Begin with walking, progress gradually with medical clearance
- Listen to your body and adjust as needed

Essential Recovery Products
The right tools can transform your recovery experience from challenging to manageable. Thoughtfully designed products like the Sleep Again Pillow System weren't just created for convenience—they were born from the real needs of women on this same journey, addressing specific challenges with practical, comfort-focused solutions.
The Sleep Again Pillow System
-
Comprehensive design with two wedges, two body pillows, and a neck pillow
-
Multiple configurations for different recovery stages
-
Provides stable elevation to reduce swelling and pressure
-
Prevents rolling onto surgical sites during sleep
-
Offers long-term value beyond the recovery period
Additional Helpful Products
-
Front-closing shirts and pajamas
-
Drain management items
-
Shower chair or bench
-
Reacher/grabber tool
-
Gentle skin care products
Long-term Follow-up Care
Recovery extends beyond the initial healing phase into a lifetime of mindful health monitoring. Regular follow-up care becomes your new normal—not from a place of fear, but from a commitment to your continued wellbeing. These check-ins are celebrations of your survivorship and opportunities to address any concerns promptly.
Typical Follow-up Schedule
-
More frequent visits in the first year
-
Gradually extending intervals between appointments
-
Regular imaging of remaining breast tissue if applicable
Self-Monitoring
-
Monthly self-examination of chest wall
-
Awareness of normal sensation in the surgical area
-
Monitoring for lymphedema if lymph nodes were removed
When to Contact Your Healthcare Team
-
New lumps or skin changes in the surgical area
-
Persistent pain that differs from your usual pattern
-
Swelling in your arm, hand, or chest
-
Emotional distress that interferes with daily functioning
Living Well Beyond Mastectomy
This surgery may be part of your story, but it doesn't define your entire narrative. Beyond recovery lies a life rich with possibility and meaning. Many women discover unexpected gifts in this journey—deeper appreciation for life, stronger connections, and newfound resilience. Your "after" can be even more meaningful than your "before."
Finding Your New Normal
-
Acknowledge both challenges and strengths discovered during recovery
-
Recognize how priorities may have shifted
-
Focus on what you've gained as well as what you've lost
Physical Wellness Beyond Recovery
-
Maintain a sustainable exercise routine
-
Continue using the Sleep Again Pillow System for optimal sleep
-
Address any lingering physical issues rather than accepting them as permanent
Wisdom from the Journey
-
Patience with the recovery process is essential
-
The value of asking for and accepting help
-
The importance of quality rest for healing
-
The discovery of unexpected strength and resilience
Remember that healing is not linear, and there is no timeline by which you "should" feel or function in certain ways. Be gentle with yourself, celebrate your progress, and know that each day brings new opportunities for healing and wellness.
This guide aims to support you through mastectomy recovery with information drawn from medical expertise and personal experiences. Always consult with your healthcare team about your individual recovery plan.
The Sleep Again Pillow System mentioned throughout this guide has been specifically designed to address the unique sleep and comfort challenges faced during mastectomy recovery. Its comprehensive approach—with wedges, body pillows, and neck support—offers versatile positioning options for each phase of healing.