You've taken the important step toward better breathing with septoplasty surgery—now comes the recovery challenge that catches most patients off guard. Sleeping comfortably while your newly restructured nasal passages heal can feel impossible, especially when every position you've relied on for years suddenly works against your recovery rather than supporting it.
If you're discovering that post-septoplasty sleep requires more strategy than you expected, you're not alone. Your nasal passages are swollen, potentially packed with gauze, and your entire sinus system is running a healing program with very specific requirements. The comfortable sleep positions you've counted on may be temporarily off-limits, but that doesn't mean you have to suffer through weeks of poor rest.
The encouraging news? Septoplasty sleep challenges have proven solutions. This isn't about enduring discomfort until things improve—it's about understanding exactly what your healing sinuses need and creating the optimal conditions to support both quality rest and faster recovery.
Ready to transform your post-surgery bedroom into a healing sanctuary? Let's explore the medically-backed positioning strategies that turn sleep into an active part of your recovery process.
Understanding Your Post-Septoplasty Body
Septoplasty fundamentally changes how your nasal and sinus systems function, creating a cascade of temporary adjustments that affect every aspect of sleep. Your surgeon has straightened your deviated septum, but your body now needs time to adapt to improved airflow patterns while healing from the surgical intervention.
The physiological changes you're experiencing:
Altered airflow dynamics: Your nasal passages are learning to process air through newly opened pathways. This adjustment period can create unusual sensations, temporary congestion despite surgical improvement, and changes in how air moves through your sinuses during different sleep positions.
Inflammatory response management: Your immune system is actively healing surgical sites while managing normal post-operative inflammation. This process affects tissue swelling, drainage patterns, and sensitivity levels throughout your upper respiratory system.
Nerve pathway adaptation: Septoplasty can temporarily affect nerve pathways in your nasal area, leading to changed sensation patterns, altered pain perception, and different responses to positional pressure than you experienced before surgery.
Mucus production changes: Your sinuses are recalibrating their normal mucus production and clearance patterns, which can affect drainage, breathing comfort, and the effectiveness of different sleeping positions during recovery.

The Science Behind Elevated Sleep Positioning
Medical professionals consistently recommend elevated back sleeping at 30-45 degrees for septoplasty recovery because this position optimizes multiple physiological processes simultaneously. Understanding the scientific rationale helps you commit to positioning that may initially feel unfamiliar.
Gravitational Drainage Physics
The elevated angle works with Earth's gravity to create optimal fluid dynamics within your healing sinuses. When positioned correctly, gravity assists your lymphatic system in moving inflammatory fluids away from surgical sites, prevents pooling of healing secretions in dependent areas, and maintains clear drainage pathways that reduce infection risk.
The 30-45 degree sweet spot: Research shows that angles below 30 degrees don't provide sufficient gravitational assistance, while angles above 45 degrees can create neck strain and cause patients to slide down during sleep, losing therapeutic benefits.
Cardiovascular Benefits During Recovery
Elevation reduces the workload on your cardiovascular system during the energy-intensive healing process. Your heart doesn't have to work as hard to maintain circulation to your head and face, blood return from your extremities improves, and overall circulation efficiency increases, delivering more healing nutrients to surgical sites.
Respiratory Mechanics Optimization
Even with restricted nasal breathing, elevated positioning helps optimize your respiratory function by naturally opening airways, reducing the work required for each breath, improving lung expansion patterns, and supporting better oxygen exchange—all crucial for healing tissue repair.
Pain Management Enhancement
Proper elevation creates more comfortable pressure distribution across your face and head, reducing concentrated pressure on sensitive post-surgical areas, improving the effectiveness of pain medications, and promoting longer periods of uninterrupted sleep necessary for optimal healing.
Your Comprehensive Recovery Timeline
Understanding what to expect during each phase of recovery helps you adjust your sleep strategies appropriately and recognize normal healing progress.
Days 1-3: Acute Recovery Phase
This initial period represents the most challenging sleep phase, when your body is managing peak inflammation and your nasal passages are most restricted.
Physiological changes: Maximum tissue swelling, peak inflammatory response, most restricted airflow, highest pain levels, and potential presence of nasal packing or splints.
Sleep characteristics: Expect 3-5 hours of fragmented sleep, frequent wake-ups for nasal care, significant mouth breathing dependency, and possible medication-related sleep disruption.
Positioning requirements: Strict 40-45 degree elevation, no deviation from back sleeping, maximum drainage support, and consistent positioning throughout the night.
Breathing support strategies: Use prescribed humidification consistently, maintain optimal room temperature (65-68°F), keep emergency supplies within reach, and follow prescribed medication schedules precisely.
Days 4-7: Stabilization Phase
Your body begins adapting to healing changes while inflammation starts decreasing noticeably.
Physiological improvements: Reduced tissue swelling, decreased inflammatory response, gradual improvement in nasal airflow, and better pain control with medication.
Sleep progression: Achieve 4-6 hours of sleep with fewer interruptions, reduced frequency of repositioning needs, less dependence on mouth breathing, and improved comfort in elevated positions.
Positioning adjustments: May reduce elevation to 35-40 degrees if comfortable, maintain back sleeping as primary position, and begin testing stability of your positioning system.
Recovery milestones: Notice easier breathing during certain times of day, experience less morning facial stiffness, and find your positioning setup becoming more familiar and comfortable.
Week 2: Adaptation Phase
Your body continues healing while beginning to adapt to improved nasal function.
Physiological developments: Significant reduction in swelling, improved sinus drainage patterns, return of some nasal breathing capacity, and decreased sensitivity in surgical areas.
Sleep quality improvements: Extend sleep periods to 5-7 hours, experience fewer wake-ups for discomfort, begin enjoying more restorative sleep phases, and notice improved morning energy levels.
Positioning flexibility: Experiment with reducing elevation to 30-35 degrees, test brief periods of side positioning (with surgeon approval), and maintain protective back sleeping as primary position.
Breathing enhancements: Notice improved airflow during certain activities, experience less morning congestion, and find humidification needs becoming less critical.
Weeks 3-4: Integration Phase
Your body integrates healing improvements while preparing for expanded positioning options.
Healing progress: Substantial reduction in post-surgical inflammation, near-normal sinus drainage patterns, significant improvement in nasal breathing, and reduced pain levels.
Sleep normalization: Achieve 6-8 hours of regular sleep, wake up feeling more rested, experience fewer positioning-related disruptions, and begin approaching pre-surgery sleep quality.
Position expansion: Carefully introduce supported side sleeping, reduce elevation angles based on comfort, and test tolerance for varied positions with medical approval.
Functional improvements: Notice improved breathing during physical activity, experience better sleep efficiency, and find less dependence on positioning aids.
Month 2 and Beyond: Optimization Phase
Your body completes primary healing while optimizing the benefits of surgical improvement.
Long-term adjustments: Complete resolution of surgical inflammation, full adaptation to improved nasal function, normal sinus drainage patterns, and optimal breathing capacity.
Sleep restoration: Return to near-normal sleep patterns, achieve pre-surgery sleep quality or better, experience minimal positioning restrictions, and enjoy improved overall sleep health.
Position freedom: Graduate to preferred sleep positions with medical clearance, maintain beneficial positioning habits learned during recovery, and use elevation strategically for ongoing sinus health.

Professional Positioning Systems for Better Sleep After Septoplasty
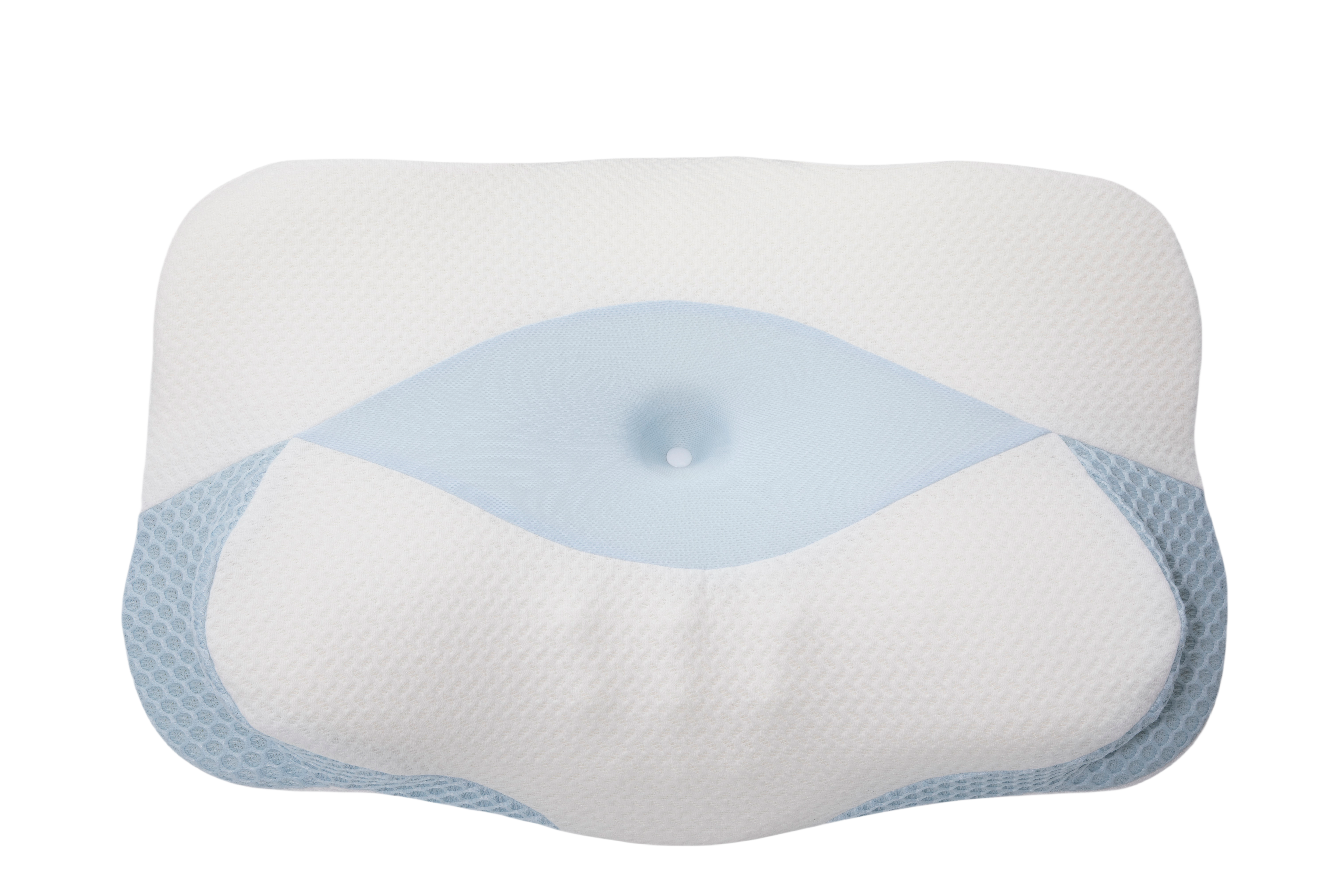
While comprehensive sleep positioning can be achieved through various methods, professional systems offer engineered solutions that eliminate common challenges. The Sleep Again Pillow System represents the gold standard in post-surgical positioning, featuring a patented 5-piece design specifically created for recovery needs.
This integrated system maintains a therapeutic 30-45 degree elevation consistently throughout the night, provides comprehensive body support that prevents rolling and maintains spinal alignment, and offers HSA/FSA qualified medical expense status. The system eliminates the trial-and-error process common with DIY positioning approaches while providing the stability and consistency that septoplasty recovery requires.
Every Sleep Again Pillow System includes:
-
Two Contoured Side Pillows to cradle the back and hips
-
Upper Body Wedge to create optimal upper body incline
-
Leg Support Wedge to gently elevate legs
-
Head Pillow to provide head support and neck mobility
-
Removable, washable slipcovers for every piece
SHOP THE BEST PILLOW FOR SEPTOPLASTY RECOVERY
Dealing with Sleep Position Anxiety
Many patients develop anxiety about maintaining proper positioning throughout the night.
Building confidence: Start with shorter rest periods in elevated positions during the day, practice positioning setup when alert and comfortable, and create consistent bedtime routines that become automatic.
Managing position fears: Understand that brief position changes won't harm healing, focus on general positioning principles rather than perfect angles, and trust that your body will adapt to beneficial positions over time.
 Frequently Asked Questions
Frequently Asked Questions
Q: How long will I need to sleep elevated after septoplasty?
A: Most patients require 4-6 weeks of elevated sleeping, though individual healing varies. Your surgeon will provide specific timelines based on your progress, procedure complexity, and healing response.
Q: Why does my face hurt more when lying flat?
A: Flat positioning increases blood flow to your head and face, worsening post-surgical swelling and pressure. Elevation uses gravity to reduce these effects naturally.
Q: Is it normal to have virtually no nasal breathing initially?
A: Yes, complete nasal congestion is expected for 1-2 weeks due to surgical swelling, potential packing materials, and normal inflammatory response.
Q: Can I sleep on my side after septoplasty?
A: Side sleeping is typically discouraged for 2-3 weeks to optimize drainage and prevent pressure on healing tissues. Your surgeon will advise when side sleeping becomes appropriate.
Q: What's the optimal room temperature for recovery sleep?
A: Maintain 65-68°F to support comfortable sleep while managing post-surgical inflammation. Slightly cooler temperatures often feel more comfortable during recovery.
Q: How do I know if my drainage is normal?
A: Normal drainage is clear to light yellow and gradually decreases. Contact your surgeon for thick, colored, foul-smelling, or increasing discharge.
Q: Should I use a humidifier throughout recovery?
A: Yes, maintaining 40-50% humidity helps prevent excessive drying of healing nasal tissues and supports more comfortable mouth breathing.
Q: When can I return to stomach sleeping?
A: Stomach sleeping typically returns last, often 6-8 weeks post-surgery, as this position can interfere with drainage and pressure healing tissues.
Q: Is it worth investing in professional positioning equipment?
A: Professional systems like the Sleep Again Pillow System provide consistent therapeutic positioning from night one and often continue benefiting sleep quality long after recovery.
Q: What should I do if elevation makes my back uncomfortable?
A: Ensure you have leg support to maintain proper spinal alignment, use pillows that maintain their shape rather than compressing, and consider professional positioning systems designed for extended elevated sleep.
When to Contact Your Medical Team
Certain symptoms require immediate medical attention regardless of positioning effectiveness:
-
High fever (over 101°F) that doesn't respond to medication
-
Sudden severe headache or facial pain that worsens despite proper elevation
-
Vision changes or significant eye swelling
-
Bright red bleeding that doesn't stop with gentle pressure
-
Signs of infection including increasing redness, warmth, or foul-smelling drainage
-
Difficulty swallowing or breathing that worsens rather than improves
-
Persistent vomiting that prevents medication or fluid intake
Remember that optimal positioning supports your recovery but doesn't replace necessary medical monitoring and intervention when complications arise.
Your Path to Recovery Success
Septoplasty recovery sleep follows predictable patterns, and understanding these phases helps you navigate the process with confidence. Elevated back sleeping at 30-45 degrees isn't merely a comfort suggestion—it's a therapeutic intervention that directly supports faster healing and better outcomes.
Whether you choose carefully arranged household pillows or invest in a professionally designed system like the Sleep Again Pillow System, the goal remains consistent: creating sustainable elevation that works night after night throughout your recovery.
Most importantly, this challenging period is temporary. You will return to normal sleep patterns, and you'll breathe significantly better than before surgery. The positioning commitment you're making now directly invests in long-term breathing improvement and enhanced sleep quality for years to come.
Quality sleep during septoplasty recovery isn't a luxury—it's a medical necessity that directly affects healing speed and completeness. Trust the process, give your body the positioning support it needs, and look forward to the improved breathing and sleep quality that awaits you.
Medical Disclaimer
This information is provided for educational purposes only and should not replace professional medical advice. Every septoplasty procedure and recovery process is unique, and sleeping position recommendations may vary based on your specific surgical approach, individual health conditions, and post-operative circumstances.
Always follow your surgeon's specific post-operative instructions regarding sleep positioning, nasal care, activity restrictions, and recovery protocols. These medical guidelines take precedence over any general positioning advice provided here.
Contact your healthcare provider immediately if you experience concerning symptoms such as high fever, severe pain, vision changes, excessive bleeding, or signs of infection. If you have persistent sleep problems that significantly impact your recovery, discuss these with your medical team rather than attempting to self-treat with positioning changes alone.