If you've just been diagnosed with shingles, you have a critical window of opportunity to prepare for one of the most challenging aspects of recovery: nighttime pain intensification. Understanding what's coming and setting up proper support systems now—before symptoms peak—can make the difference between sleepless nights and restorative rest.
Here's what you need to know: shingles pain doesn't stay constant throughout the day. The nerve discomfort that feels manageable during your diagnosis appointment will likely intensify dramatically during evening and nighttime hours. This isn't a sign of complications or treatment failure—it's a predictable, well-documented response based on how your body's natural pain control systems operate.
The good news? You can take action right now to minimize this nighttime intensification. By understanding the mechanisms behind nocturnal pain increases and implementing strategic positioning and environmental modifications before your symptoms peak, you'll be equipped to maintain the quality sleep your immune system desperately needs to fight the viral infection effectively.
This preparation isn't just about comfort—it's about optimizing your recovery. Your body relies on deep sleep phases to mount an effective immune response against the shingles virus. Setting up proper nighttime positioning and pain management strategies now, while you still have the energy and mobility to do so, is a medical necessity that directly impacts how quickly and completely you'll recover.
The Science Behind Nighttime Shingles Pain Intensification
Your Body's Natural Pain Control System
Your pain management system operates on a 24-hour cycle that directly affects how intensely you experience shingles discomfort. During daylight hours, your adrenal glands produce peak levels of cortisol—a natural anti-inflammatory hormone that suppresses pain signals and reduces nerve inflammation.
As evening approaches, cortisol production naturally declines as part of your circadian rhythm preparation for sleep. This reduction in natural pain-fighting hormones occurs precisely when you need relief most, leaving inflamed nerve pathways from the shingles virus more vulnerable to pain signal transmission.
The Distraction Factor
During active daytime hours, your brain processes multiple competing stimuli—work tasks, conversations, visual input, and physical activities. This cognitive load provides natural distraction from pain signals, effectively reducing their perceived intensity through divided attention mechanisms.
When you prepare for sleep and your environment becomes quiet, these competing stimuli disappear. Your brain's processing capacity becomes available to focus on pain signals that were previously competing for attention, making the same level of discomfort feel more intense.
Physical Position Changes
The transition from upright to horizontal positioning creates changes that can intensify shingles pain. Blood flow patterns shift when lying down, potentially increasing pressure around inflamed nerve pathways. Contact between affected skin areas and bedding materials can trigger pain responses in hypersensitive nerve endings, creating new sources of discomfort right when you're trying to achieve rest.
Understanding Different Types of Shingles-Related Pain
Acute Neuralgic Pain
This sharp, electric-shock-like pain follows specific nerve pathways during active shingles outbreaks. It typically intensifies during the first 1-2 weeks when viral replication is most active and nerve inflammation peaks.
Post-Herpetic Neuralgia
Approximately 10-15% of shingles patients develop chronic nerve pain that persists after visible lesions heal. This deep, burning, or aching pain can continue for months or years, requiring different management strategies than acute phase pain.
Touch Sensitivity (Allodynia)
Many shingles patients develop hypersensitivity where normally painless stimuli—light touch, clothing contact, or air movement—trigger intense pain responses. This complicates nighttime positioning because contact with bedding becomes problematic.

Strategic Approaches to Nighttime Shingles Relief
Environmental Optimization
Temperature Control: Maintain bedroom temperatures between 65-68°F. Heat can intensify nerve pain, while cooler environments may provide relief. Use breathable bedding materials that prevent heat retention around affected areas.
Surface Selection: Choose smooth, soft fabrics that minimize friction against sensitive skin. Bamboo and silk materials typically cause less irritation than cotton or synthetic blends. Consider placing smooth barriers between affected skin and bedding to prevent direct contact while allowing air circulation.
Lighting Management: Use dim, warm lighting in the evening to support natural sleep preparation while providing adequate visibility for medication application and positioning setup.
The Power of Therapeutic Elevation
Proper positioning during shingles recovery addresses multiple pain factors simultaneously. Elevation at 30-45 degrees reduces direct contact pressure on affected areas, improves circulation around inflamed nerve pathways, and minimizes the need for frequent position changes that can disrupt rest.
The key challenge is maintaining consistent therapeutic positioning throughout the night without the shifting and compression that occurs with standard household pillows. Regular pillows compress under body weight and lose their supportive angles within hours, leaving you without the relief you need most.

Professional Positioning Solutions for Nighttime Shingles Pain
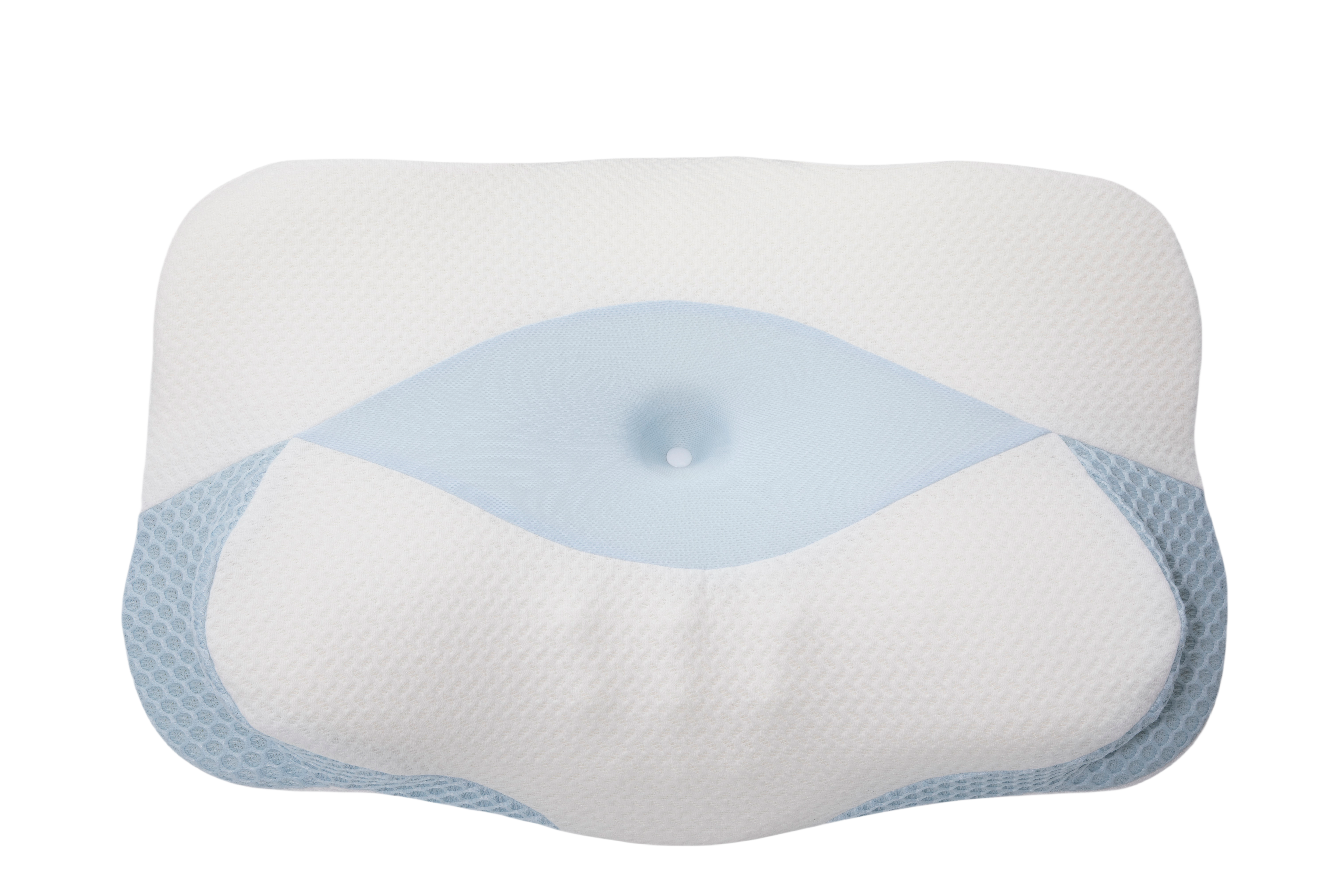
The Sleep Again Pillow System addresses the specific positioning challenges that shingles patients face during recovery. Unlike consumer comfort pillows, this system maintains therapeutic angles consistently throughout extended sleep periods.
Every Sleep Again Pillow System includes:
-
Two Contoured Side Pillows to cradle back and hips
-
Upper Body Wedge to create optimal upper body incline
-
Leg Support Wedge to gently elevate legs
-
Head Pillow to provide head support and neck mobility
-
Removable, washable slipcovers for every piece
Clinical advantages for shingles patients:
Consistent elevation maintenance: The Upper Body Wedge provides stable 30-45 degree positioning that doesn't compress or shift during sleep, ensuring continuous pressure relief for affected areas throughout the night.
Integrated support architecture: The components work together to support your entire body in the elevated position, preventing gaps or pressure points that can worsen nerve pain while accommodating normal sleep movement.
Medical equipment durability: Advanced construction materials maintain positioning properties throughout extended use periods, providing reliable therapeutic benefits that justify the investment over weeks or months of recovery.
Treatment compatibility: The stable positioning works with topical treatments and doesn't interfere with wound care or medication application routines, supporting your complete treatment protocol.
SHOP THE BEST PILLOW FOR SHINGLES PAIN RELIEF
Comprehensive Pain Management Strategies
Medication Timing Optimization
Work with your healthcare provider to optimize medication schedules for nighttime relief. Apply prescribed topical treatments 30 minutes before bed to allow adequate absorption time. Take pain medications 45 minutes before your target sleep time to ensure peak effectiveness during initial sleep phases.
Early antiviral treatment significantly impacts the severity and duration of shingles outbreaks. These medications work best when started within 72 hours of symptom onset and maintained at consistent blood levels throughout the treatment period.
Non-Pharmaceutical Relief Methods
Cool compress therapy: Use cool compresses on affected areas for 15-20 minutes before bed, then remove them before getting into positioned sleep setup. The cooling sensation can temporarily interrupt pain signals and reduce local inflammation.
Stress reduction techniques: Implement relaxation strategies that work within your positioning requirements. Focus on controlled breathing exercises, progressive muscle relaxation avoiding affected areas, and audio distraction through guided meditation recordings at low volumes.
Sleep aid considerations: Temporary sleep aids may be appropriate during the acute phase when pain significantly disrupts rest, but should be used strategically rather than routinely.
Recovery Timeline and Positioning Adaptation
Acute Phase Management (Days 1-14)
During active blister formation and peak pain intensity, focus on maximum protection and comfort. This is when proper positioning provides the most significant relief by minimizing contact with affected areas and supporting optimal circulation.
Priority strategies include consistent therapeutic elevation at 35-45 degrees, stable positioning that doesn't require frequent adjustments, cool environment maintenance, and gentle topical treatment application before positioning.
Healing Transition (Weeks 3-6)
As acute symptoms subside and lesions begin healing, you can gradually modify positioning while monitoring for signs of post-herpetic neuralgia development. Consider gradual reduction of elevation angles as comfort improves, assessment of ongoing sensitivity patterns, and position variation introduction based on healing progress.
Long-term Recovery (Months 2+)
Most patients achieve significant improvement during this period, though some develop chronic symptoms requiring ongoing management approaches. Continue monitoring for persistent pain patterns and adapt positioning strategies based on evolving needs.

Investment Analysis: Professional vs. DIY Solutions
Cost-Effectiveness Comparison
DIY pillow approaches typically involve multiple purchases ($100-200 for various types), replacement costs as pillows compress and lose effectiveness ($50-100), and significant time investment (15-20 minutes nightly for setup and adjustment) with variable effectiveness requiring frequent modification.
Professional positioning systems like the Sleep Again Pillow System provide complete integrated solutions with 5-minute setup time once familiar with configuration, consistent therapeutic positioning throughout recovery periods, and long-term value that continues providing benefits beyond acute recovery phases.
Value Consideration for Shingles Recovery
For conditions affecting sleep quality over weeks or months, professional positioning equipment often provides cost-effective relief through improved rest quality and reduced need for additional comfort purchases. The investment becomes particularly valuable when considering the role of quality sleep in immune function and recovery acceleration.
SHOP THE BEST PILLOW FOR SHINGLES PAIN RELIEF
Medical Management and Warning Signs
When to Seek Immediate Care
Contact your healthcare provider immediately for shingles affecting eye or facial areas, signs of secondary bacterial infection, severe headache with neck stiffness, vision/hearing/balance changes, or weakness/numbness beyond typical shingles distribution.
Ongoing Monitoring
Schedule follow-up evaluation for pain that worsens after initial improvement, symptoms persisting beyond 6-8 weeks, development of new pain types weeks after initial outbreak, or sleep disruption that doesn't improve with positioning strategies.
Frequently Asked Questions
Q: How long does nighttime shingles pain typically last?
A: Most acute nighttime pain improves significantly within 2-4 weeks as the viral outbreak resolves. However, some patients develop post-herpetic neuralgia, which can cause persistent nighttime discomfort for months or longer.
Q: Should I sleep sitting up if lying down is too painful?
A: Some patients find temporary relief in recliners during severe acute phases. However, chairs rarely provide the comprehensive support needed for quality restorative sleep. Proper elevation in bed using systems like the Sleep Again Pillow System typically provides better long-term comfort and sleep quality.
Q: Can poor sleep make my shingles outbreak worse?
A: Sleep deprivation can impair immune function and potentially prolong viral activity, making effective sleep positioning crucial for optimal recovery.
Q: Why does gentle touch hurt more than firm pressure?
A: This condition, called allodynia, occurs when damaged nerves misinterpret light touch as painful stimuli. Firm pressure activates different nerve pathways that don't trigger the same pain response.
Q: How do I know if I need professional positioning equipment?
A: If you're experiencing significant sleep disruption due to shingles pain or finding that DIY pillow arrangements don't provide stable relief, professional positioning systems often provide immediate improvement that justifies the investment.
Q: Will elevation help with both pain and itching?
A: Proper elevation can help reduce local inflammation, which may decrease both pain and itching intensity. However, itching often requires specific treatments like antihistamines or prescribed topical preparations in addition to positioning strategies.
Q: Can I use regular pillows along with positioning equipment?
A: Professional positioning systems like the Sleep Again Pillow System are designed to provide complete support independently. Adding regular pillows often creates instability and pressure points that can worsen comfort.
Q: How do I maintain proper positioning if I move during sleep?
A: Quality positioning systems are designed to accommodate normal sleep movement while maintaining therapeutic angles. Integrated components work together to provide stable support even with minor position changes during sleep cycles.
Q: What's the difference between positioning for shingles versus other conditions?
A: Shingles positioning focuses specifically on reducing contact pressure on hypersensitive nerve areas while maintaining therapeutic elevation, which differs from post-surgical positioning that emphasizes incision protection.
Q: Should I continue elevation after my shingles symptoms resolve?
A: Many patients find that the improved sleep quality from proper elevation provides ongoing benefits beyond shingles recovery, supporting general sleep health and comfort long after acute symptoms resolve.
The Path to Better Nights
Nighttime shingles pain represents a temporary but significant challenge that responds well to targeted intervention strategies. Understanding the biological mechanisms behind increased nocturnal symptoms enables you to implement evidence-based solutions rather than hoping for spontaneous improvement.
The most effective approach combines environmental optimization, therapeutic positioning, appropriate medical treatment, and realistic expectations about recovery timelines. Professional positioning solutions like the Sleep Again Pillow System provide immediate, consistent relief that often proves more cost-effective than multiple temporary measures over the recovery period.
Recognize that shingles recovery, while challenging, follows predictable patterns. The acute phase will resolve, pain levels will decrease, and normal sleep patterns will return. However, getting adequate rest during the recovery process significantly impacts both your immediate comfort and long-term outcomes.
Don't hesitate to invest in tools and strategies that improve your sleep quality during this challenging period. Your recovery depends on restorative sleep, and proper positioning provides the foundation for achieving that rest despite temporary nerve pain challenges.
Medical Disclaimer
This information is provided for educational purposes only and should not replace professional medical advice. Shingles (herpes zoster) is a serious viral infection requiring proper medical evaluation, diagnosis, and treatment by qualified healthcare providers.
The symptoms, severity, duration, and complications of shingles vary significantly among individuals based on factors including age, immune system status, outbreak location, and treatment timing. Always consult with your healthcare provider before implementing new pain management strategies or positioning techniques.
Seek immediate medical attention for concerning symptoms including vision changes, severe headache with neck stiffness, signs of bacterial infection, or neurological symptoms beyond typical shingles distribution. Early medical intervention can significantly impact outcomes and reduce complication risks.
Post-herpetic neuralgia and other chronic complications require specialized medical management. If pain persists beyond the acute phase or new symptoms develop weeks after initial outbreak, consult your healthcare provider for evaluation and treatment options.