You're scheduled for abdominal surgery, and your surgeon mentioned the importance of rest during recovery. Sound advice, but here's what you need to know now: the position you sleep in after surgery will significantly impact how well you heal.
Planning your post-surgery sleep strategy before your procedure helps you recover more comfortably and avoid common positioning mistakes that can slow healing. When you're prepared with the right setup, you won't be scrambling to find comfortable positions while managing post-surgical pain.
Here's what you need to understand: sleep position after abdominal surgery isn't just about comfort—it's about creating optimal conditions for your body to repair itself. The right positioning reduces swelling, improves circulation, protects your incision, and allows your abdominal muscles to rest.
This guide covers the positioning strategies that support abdominal surgery recovery and how to create a sleep setup that works consistently—so you can prepare everything before your procedure.
Why Does Sleep Position Matter So Much After Abdominal Surgery?
Understanding what your body will experience after surgery helps you prepare the right positioning strategy in advance.
Your Abdominal Wall Will Be Structurally Compromised
The muscles and tissue layers that normally support your core will be temporarily weakened. Wrong positioning will create tension across these healing structures, increasing pain and potentially slowing recovery.
Inflammation Will Need Management
Post-surgical swelling is natural, but proper positioning uses gravity to encourage lymphatic drainage and reduce inflammation around your surgical site.
Gas Pain Will Be a Challenge
Many abdominal surgeries use laparoscopic techniques that pump CO2 gas into the abdomen. That gas will need to dissipate, and lying flat will trap it against your diaphragm, causing shoulder pain.
Circulation Will Affect Everything
Quality blood flow delivers oxygen and nutrients to healing tissue. The right sleep position will optimize circulation without taxing your cardiovascular system.
Core Stability Will Matter Even When Sleeping
Your abdominal muscles normally stabilize your torso. When healing from surgery, poor positioning will force these compromised muscles to work continuously, preventing needed rest.

What Is the Best Sleep Position After Abdominal Surgery?
Elevated back sleeping at 30-45 degrees will be your primary position during recovery. Planning this setup before surgery ensures you're ready when you return home.
This angle addresses the major recovery challenges you'll face.
Gas Relief Through Physics
When you're elevated, CO2 gas will naturally migrate toward areas where your body can process and eliminate it instead of settling against your diaphragm.
Pressure Distribution
Elevated positioning will spread your body weight over a larger surface area, reducing concentrated pressure on your incision.
Reduced Abdominal Tension
At 30-45 degrees, your torso will maintain a gentle bend that keeps abdominal muscles relaxed, eliminating the stretching force of lying flat.
Improved Lymphatic Drainage
Elevation creates the optimal angle for lymph to drain away from your surgical site, reducing swelling and removing inflammatory byproducts.
Enhanced Circulation
Your heart won't have to work as hard to circulate blood, meaning more efficient oxygen delivery to healing tissue.
Easier Mobility
Getting up from an elevated position will require less core muscle engagement than rising from a flat position—crucial for nighttime bathroom trips.
Finding Your Optimal Angle
This range isn't arbitrary—it's the result of understanding how gravity and healing intersect. Below 30 degrees, you don't get adequate benefits. Above 45 degrees, you'll slide down all night. The sweet spot delivers maximum therapeutic benefit while remaining sustainable.
How Should I Set Up My Bed Before Surgery?
Preparing your sleep setup before your procedure means you won't be struggling with pillows while managing post-surgical pain.
Essential Components You'll Need
Upper Body Support: Firm, stable elevation from lower back through shoulders that will hold its angle throughout the night.
Leg Elevation: A wedge under your knees (15-20 degrees of bend) will maintain spinal alignment and prevent sliding.
Lateral Support: Pillows on both sides will prevent rolling and keep your spine aligned.
Head/Neck Positioning: A separate pillow will allow neck adjustment independent of torso angle.
The DIY Pillow Approach
What You'll Need: 3-4 firm bed pillows for your upper back, a pillow for under your knees, pillows for both sides, and a final pillow for head support.
What to Expect: Standard pillows will compress significantly overnight, gradually reducing elevation. You'll likely need to adjust your setup during the night. Pillow edges can create pressure points, and the system may shift with movement.
When DIY Works: Short-term recovery (under 1 week) or limited budget.

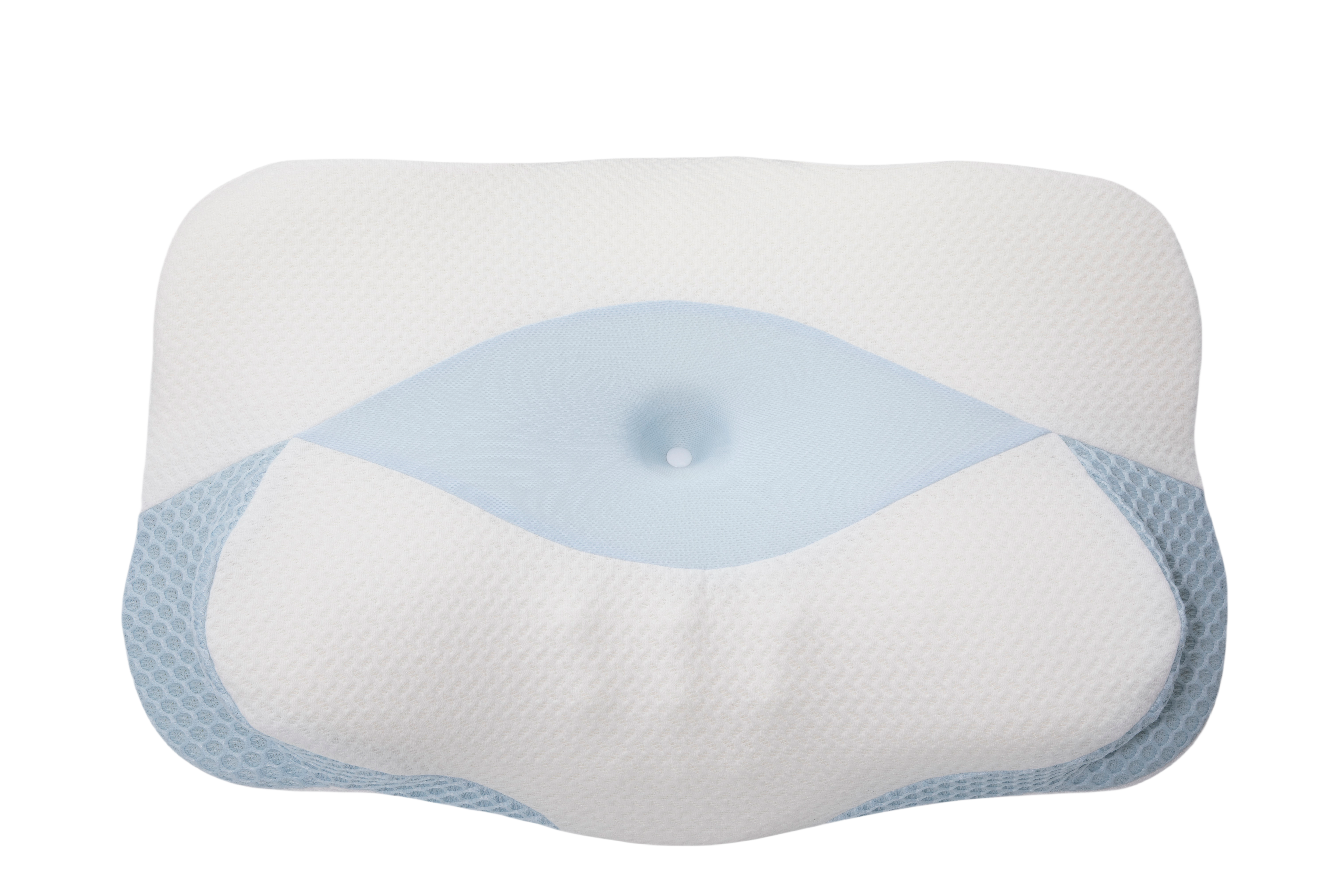
The Sleep Again Pillow System: Supporting Better Sleep After Abdominal Surgery
If you're preparing for a recovery period longer than two weeks, investing in professional-grade positioning equipment before surgery can significantly improve your comfort.
The Sleep Again Pillow System is the only full-body pillow system designed specifically for surgery support.
Every Sleep Again Pillow System includes:
-
Two Contoured Side Pillows to cradle back and hips
-
Upper Body Wedge to create optimal upper body incline
-
Leg Support Wedge to gently elevate legs
-
Head Pillow to provide head support and neck mobility
-
Pillow Straps with Clasp to keep side pillows secure
-
Removable, washable slipcovers for every piece
The system is HSA/FSA eligible, allowing you to use pre-tax medical funds. Ordering before your surgery means your positioning system will be ready when you return home—no struggling to set up pillows or making emergency purchases during recovery.
SHOP THE BEST PILLOW SYSTEM FOR ABDOMINAL SURGERY
When Can I Sleep on My Side After Abdominal Surgery?
Understanding the timeline for side sleeping helps you plan your recovery expectations.
The Two Weeks: Not Recommended
Side sleeping will create challenges during acute healing:
-
Gravity will pull abdominal contents toward your incision
-
Your torso may roll forward, stretching healing tissue
-
Core muscles will need to engage continuously
-
Circulation can become compromised without support
Week 3-4: Gradual Introduction
Once initial inflammation decreases, you'll be able to begin testing side sleeping carefully:
-
Start with your non-surgical side to minimize direct pressure
-
Prepare a support system: pillow between knees, pillow against abdomen, pillow behind back, proper head support
-
Test during the day first for 15-20 minutes before attempting overnight
-
Plan short intervals: begin in elevated back position, then transition mid-night
Signs You'll Need to Return to Back Sleeping:
-
Sharp or increasing pain at incision
-
Sensation of pulling or stretching
-
Difficulty getting comfortable within 10 minutes
-
Increased swelling the following day
When Can I Return to Stomach Sleeping After Abdominal Surgery?
If you're a stomach sleeper, plan for this position to be off-limits for the longest period.
Why Stomach Sleeping Will Require More Time:
-
Direct pressure on healing incision
-
Abdominal wall will need to support significant compressive force
-
Breathing will become more difficult
-
Spine extends backward, creating tension across abdomen
Expected Recovery Timeline:
Weeks 1-4: Not recommended during this healing phase.
Weeks 4-6: Continue avoiding unless specifically cleared by your surgeon.
Weeks 6-8: Many patients can begin testing for short 20-30 minute periods.
Week 8+: Most patients can return to stomach sleeping if pain-free and fully healed.
Your surgeon will provide specific guidance based on your procedure type.
How Should I Prepare for Sleep Disruptions After Surgery?
Pain Management Planning: Plan to take prescribed medication 30-60 minutes before bed for peak effectiveness. Set up quiet alarms for scheduled doses so you can maintain your medication schedule without fully waking.
Gas Pain Preparation: Prepare to take short walks before bed if approved by your surgeon. Have peppermint tea available. Apply gentle heat to your shoulder or upper back (not incisions). Maintain strict elevation to manage gas-related discomfort.
Bathroom Frequency Planning: Expect multiple nighttime bathroom trips. Practice getting out of bed during the day before surgery so the movement pattern becomes automatic. Install nightlights between bed and bathroom for safe navigation.
What Sleep Position Problems Should I Watch For After Surgery?
Understanding warning signs before your procedure helps you know when to contact your medical team.
Situations Requiring Immediate Medical Attention:
-
Fever over 101°F combined with sleep position problems
-
Severe, sharp pain that doesn't respond to position changes
-
Visible changes at your incision site (redness, warmth, drainage, separation)
-
Difficulty breathing that worsens in all positions
-
Leg swelling combined with calf pain (possible blood clot)
Issues to Schedule Follow-Up Discussion:
-
Pain that's getting worse instead of better after the first week
-
Inability to sleep more than 1-2 hours at a time despite trying different positions
-
New numbness or tingling that develops around your incision
-
Persistent gas pain that doesn't improve with elevation
-
Questions about advancing to different positions sooner than standard timelines

Your Week-by-Week Sleep Position Recovery Plan
Understanding what to expect helps you prepare mentally and physically before surgery.
Week 1-2: The Acute Phase
Primary Position You'll Use: Elevated back sleeping at 30-45 degrees, which can be achieved safely using the Sleep Again Pillow System.
Alternative Option: Recliner for watching TV or reading
What to Avoid: Stomach sleeping, flat back sleeping, unsupported side sleeping
What to Focus On: Gas relief, incision protection, inflammation management
Your body will be dealing with peak inflammation and gas pain. Maintaining consistent positioning during this week will be important for managing symptoms. Most patients find this the most challenging week, but proper elevation makes a significant difference in comfort levels.
Week 3-4: Early Healing
Primary Position You'll Use: Elevated back sleeping at 30-45 degrees
What You Can Test: Brief side sleeping trials during daytime
Still Avoid: Stomach sleeping, flat sleeping
What to Focus On: Maintaining progress while inflammation decreases
Acute symptoms will be improving, but your incision won't have gained significant strength yet. It will be important to continue with supportive positioning during this phase. Testing positions too early can potentially extend your recovery timeline.
Week 4-6: Progressive Transition
Primary Position You'll Use: Elevated back sleeping at 30-35 degrees
What You're Ready For: Side sleeping for portions of the night with full support
Still Avoid: Stomach sleeping, completely flat sleeping
What to Focus On: Gradual expansion of comfortable positions
Your body will be transitioning from acute healing to tissue strengthening. This will be the appropriate time to slowly expand your positioning options while maintaining core support principles. Listen to your body—if something causes discomfort, return to more supportive positioning.
Week 6+: Return to Normal
What You'll Work Toward: Decreasing elevation as tolerated
Positions You'll Expand To: Side sleeping without extensive support, testing flat sleeping
What to Approach Cautiously: Stomach sleeping if cleared by your surgeon
What to Focus On: Sustainable long-term comfort while supporting continued healing
Most patients can reduce elevation significantly by week 6, though some procedures require longer. This phase will be about finding what feels natural again while respecting your body's remaining healing needs.
SHOP THE BEST PILLOW SYSTEM FOR ABDOMINAL SURGERY
FAQ: Sleep Positions After Abdominal Surgery
How long will I need to sleep elevated after abdominal surgery?
Most patients require 2-4 weeks of elevated back sleeping, though this varies by procedure complexity. Simple procedures like appendectomy might need only 10-14 days of elevation, while complex abdominal surgeries could require 4-6 weeks. Your surgeon will provide specific guidance based on your operation. The key will be maintaining elevation consistently—occasional elevated nights won't provide the same therapeutic benefit as continuous proper positioning.
When can I sleep on the side where I had surgery?
Generally, you'll wait over 4 weeks before sleeping on your surgical side, and you'll need to use support. Sleeping on your non-surgical side can begin earlier (week 2-3) once acute inflammation decreases. When you do transition to your surgical side, you'll start with just 30-60 minutes and gradually increase duration based on your body's response.
What if I wake up on my stomach after abdominal surgery?
If you naturally roll during sleep, create physical barriers with pillows on both sides of your body before surgery. Some patients use a small pillow or folded towel against their abdomen to make stomach sleeping uncomfortable enough that they'll roll over even while asleep. Body pillows work particularly well for preventing unconscious position changes during the night.
Why will my shoulder hurt after abdominal surgery?
This will be referred pain from CO2 gas trapped near your diaphragm. The phrenic nerve (which controls your diaphragm) shares nerve pathways with your shoulder, so your brain will interpret gas irritation as shoulder pain. Proper elevation will help the gas dissipate. If shoulder pain persists beyond 10-14 days or worsens instead of improving, contact your surgeon as this could indicate other issues.
Can I use a heating pad while sleeping after abdominal surgery?
Never apply heat directly to your incision, and never fall asleep with a heating pad on due to burn risk. If using heat for muscle discomfort or gas pain, apply it for 15-20 minute periods while awake, and target areas away from your surgical site. Some patients find gentle warmth on the upper back or shoulders helps with gas-related referred pain.
How do I prevent sliding down my elevated sleep position?
A wedge under your knees will be essential—this creates a "bend" in your body that prevents sliding. Your upper body support must extend from lower back through shoulders, not just behind your shoulders. If you're still sliding, increase knee elevation slightly or check that your wedge has enough surface area.
Is it normal to sleep poorly for weeks after abdominal surgery?
Disrupted sleep is extremely common during surgical recovery. Between position restrictions, pain management schedules, bathroom trips, and general discomfort, normal sleep patterns take time to re-establish. This is temporary, though frustrating.
Most patients report significant improvement around week 3-4 as pain decreases and positioning restrictions ease. The Sleep Again Pillow System, the #1 doctor-recommended pillow system for supporting elevated back sleeping, can help you get better sleep and healing during this challenging recovery phase.
Should I buy special pillows for elevation before surgery?
Regular pillows work for short-term recovery but have significant limitations: they compress overnight, shift with movement, and create pressure points. For recovery periods longer than 2 weeks, purpose-built positioning equipment provides better results and often pays for itself through improved sleep quality.
What's the difference between sleeping elevated and sleeping on pillows?
Elevation refers to your entire torso being angled at 30-45 degrees from horizontal. Simply adding pillows behind your head won't achieve this—you'll need support from your lower back through your shoulders to create true elevation that provides therapeutic benefits. Think of it like a ramp for your entire upper body, not just propping up your head and neck.
Can sleeping position affect how my incision heals?
Yes. Poor positioning can increase tension across your incision, potentially affecting how the edges come together and heal. Proper positioning distributes forces away from your surgical site, supporting optimal healing conditions. Most incisions heal well with appropriate care and positioning.
Why will I feel more comfortable sleeping in unusual positions after surgery?
Your body will be seeking positions that minimize pressure on healing tissue and reduce pain. These positions often represent your body's instinctive attempt to optimize comfort given your limitations. As healing progresses, you'll naturally return to your preferred sleep positions. Trust your body's feedback while ensuring you're not compromising healing by adopting positions that create excessive incision tension.

Your Pre-Surgery Sleep Positioning Strategy
Preparing your sleep positioning strategy before surgery sets you up for the most comfortable recovery possible.
Elevated back sleeping at 30-45 degrees will address the major post-surgical challenges you'll face. This position supports how your body heals while providing comfort during the recovery process.
Your expected progression follows a natural pattern: you'll start with maximum elevation during acute symptoms, gradually reduce angle as healing advances, slowly test alternative positions with support, and eventually return to your natural sleep preferences.
Whether you choose DIY pillow arrangements or invest in the Sleep Again Pillow System, preparing your setup before surgery means one less thing to worry about during recovery. The difference lies in how much time you'll spend adjusting pillows versus actually sleeping.
Most importantly, understand that sleep disruption during surgical recovery is temporary. Your body will be performing remarkable healing work, and positioning that supports this process is worth the preparation. You will sleep normally again, even when it feels challenging during recovery.
Prepare your sleep setup, discuss positioning with your surgeon, and consider investing in proper positioning equipment before your procedure. Quality sleep isn't a luxury—it's a medical necessity that directly affects healing speed and recovery completeness.
SHOP THE BEST PILLOW SYSTEM FOR ABDOMINAL SURGERY
Medical Disclaimer
This information is provided for educational purposes only and should not replace professional medical advice from your surgical team. Mastectomy procedures vary significantly in technique, extent, and individual patient factors that affect recovery timelines.
Always follow your surgeon's specific post-operative instructions regarding sleep positioning, physical activity restrictions, and recovery milestones. These medical guidelines take precedence over any general information provided here.
Contact your healthcare provider immediately if you experience signs of complications, including fever, sudden increase in pain, wound drainage, significant swelling, or breathing difficulties during recovery. Your surgical team knows your specific case and can provide guidance appropriate to your individual situation.
The mention of specific products is for informational purposes only and does not constitute medical endorsement. Consult your surgical team about positioning support options appropriate for your recovery needs. Every patient's recovery is unique, and equipment that works well for one patient may not be suitable for another based on individual medical factors.