After mastectomy surgery, most patients want to know when they can return to their preferred side-sleeping position.
The timeline for returning to side sleeping isn't one-size-fits-all. Your return depends on your specific surgery type, whether you had reconstruction, and how your incisions are healing. For lifelong side sleepers, weeks of mandatory back sleeping affects sleep quality, which impacts everything from pain management to emotional adjustment.
Here's the reality: Your doctor requires back sleeping initially for medical healing. Then when you're cleared to side sleep, it isn’t necessarily easy. Your chest is tender, incisions are sensitive, and the mattress creates pressure exactly where you can't tolerate it. The gap between "you're allowed to side sleep" and "side sleeping feels comfortable" is where most patients struggle—and where proper support makes all the difference.
This guide provides the medical timeline for safe side sleeping after different types of mastectomy and addresses how to make that transition comfortable when your chest tissue is still healing.
Understanding the Medical Timeline: When Side Sleeping Becomes Safe
The timeline for returning to side sleeping varies dramatically based on your specific surgical procedure. Understanding these distinctions helps you plan realistic expectations and avoid the frustration of comparing your timeline to someone whose surgery was fundamentally different from yours.
Lumpectomy: The Shortest Restriction Period
Timeline: 2-3 weeks of modified positioning, with careful side sleeping often permitted around week 3
Lumpectomy patients face the shortest restrictions because surgery removes localized tissue rather than entire breasts. Most patients can begin experimenting with side sleeping around week 3, starting with their non-operated side.
Progression for lumpectomy patients:
-
Weeks 1-2: Elevated back sleeping to reduce swelling
-
Week 3: Careful side sleeping on non-operated side with chest support
-
Week 4-6: Gradual return to operated-side sleeping
-
Week 6+: Return to normal sleeping positions
Single Mastectomy: Protecting One Side While Utilizing the Other
Timeline: 3-4 weeks before non-operated side sleeping, 8-12 weeks before operated-side sleeping
Single mastectomy creates an asymmetric recovery where your non-operated side remains unaffected. However, sleeping on that side still requires proper support to prevent your operated breast from pulling or experiencing pressure.
The non-operated side offers your first escape from back sleeping around weeks 3-4, once drains are removed and incisions show proper healing. The challenge is that your body naturally wants to roll toward your operated side during sleep—exactly what you need to prevent.
Single mastectomy progression:
-
Weeks 1-3: Strict elevated back sleeping
-
Weeks 3-4: Introduction of non-operated side sleeping with comprehensive support
-
Weeks 8-12: Careful experimentation with operated-side sleeping
-
Week 12+: Most patients can sleep on both sides with proper support
Double Mastectomy: The Longest Road Back to Side Sleeping
Timeline: 8-12 weeks before attempting any side sleeping
Double mastectomy patients face the most restrictive timeline because both sides require simultaneous protection. There's no "good side" to favor, and any side sleeping puts pressure on healing tissue.
Research shows that patients who attempt side sleeping before week 8 experience significantly higher rates of incision complications and healing setbacks. The extended timeline protects your bilateral recovery.
Double mastectomy progression:
-
Weeks 1-6: Exclusive elevated back sleeping
-
Weeks 6-8: Continued back sleeping with possibly reduced elevation
-
Weeks 8-10: First careful side-sleeping trials with comprehensive support
-
Weeks 10-12: Gradual expansion based on comfort
-
Week 12+: Most patients tolerate side sleeping with proper support
Mastectomy with Immediate Reconstruction: Complex Variables
Timeline: 10-16 weeks depending on reconstruction type
Reconstruction dramatically extends your timeline and introduces variables that make standard recommendations difficult.
Tissue expander reconstruction: Side sleeping becomes complicated because expanders create internal pressure that changes weekly. Most surgeons recommend avoiding side sleeping until expanders are fully expanded—typically 12-16 weeks minimum.
Direct-to-implant reconstruction: Timeline resembles double mastectomy at 10-12 weeks, with added considerations about implant positioning. Early side sleeping can contribute to malposition.
Flap reconstruction (DIEP, TRAM, latissimus dorsi): The longest restrictions at 12-16 weeks or more. These procedures require protecting both reconstruction and donor sites, and side sleeping can compromise blood flow during critical healing.
Why Your Surgeon Restricts Side Sleeping After Mastectomy
Understanding the medical reasoning behind restrictions helps you appreciate why following guidelines protects your long-term results. These restrictions aren't arbitrary—they're based on healing physiology and complication prevention data.
Incision Integrity and Tension Management
Side sleeping introduces lateral tension across incision lines that back sleeping doesn't create. When you sleep on your side, gravity pulls tissue toward the mattress, creating shearing forces that can interfere with proper wound healing and potentially cause wound separation, increased scarring, or delayed healing.
Incisions heal through a complex process involving inflammation, proliferation, and remodeling phases. During the first 6-8 weeks, incision strength is significantly compromised compared to uninjured tissue. The collagen fibers forming your new scar tissue are still organizing and strengthening. Premature mechanical stress from side sleeping can disrupt this organization, leading to wider scars, wound dehiscence, or prolonged healing timelines.
Drain Management and Lymphatic Considerations
Side sleeping can kink drain tubing and reduce drainage efficiency, increasing seroma risk. Additionally, mastectomy often disrupts your lymphatic system through node removal. Back sleeping with elevation optimizes lymphatic drainage through gravity, while side sleeping can impede flow and contribute to swelling complications.
The lymphatic system doesn't have a pump like your cardiovascular system—it relies on muscle contractions, breathing movement, and gravitational assistance. When lymph nodes are removed or damaged during surgery, your body must develop alternate drainage pathways. This process takes weeks to months. During this critical period, positioning significantly affects drainage efficiency and overall lymphedema risk.
Implant and Expander Positioning
For reconstruction patients, early side sleeping can contribute to implant malposition or capsular contracture requiring revision surgery. Implants and expanders need 8-16 weeks to develop stable positioning within chest tissue, and premature side sleeping can influence this critical development period.
During the initial weeks after implant placement, your body forms a capsule (scar tissue pocket) around the implant. The position you maintain during this capsule formation directly influences where the implant ultimately settles. Side sleeping too early can encourage capsule formation that positions the implant laterally or inferiorly from the intended placement, creating asymmetry that may require surgical correction.
The Side Sleeping Transition Challenge: When Medical Clearance Doesn't Mean Pain-Free Sleep
Even with medical clearance, transitioning from required back sleeping to side sleeping can be genuinely painful for most patients. This is the period where most patients struggle—your surgeon says you CAN side sleep, but the actual experience is more painful than expected.
Your doctor required back sleeping for good medical reasons during initial healing. But now that you're cleared to side sleep, your chest is still tender, incisions remain sensitive, and the pressure of lying on your side creates discomfort that standard pillows can't address. The gap between permission and comfort is where recovery support becomes essential.
Residual Tenderness and Sensitivity
Medical clearance comes when incisions can safely tolerate the position—not when it feels completely comfortable. Incision sites remain tender and hypersensitive for months after clearance. Nerve regeneration creates unpredictable sensations where some areas are numb while adjacent areas are hypersensitive.
The healing process involves multiple layers of tissue repair. Surface incisions may look healed while deeper tissue continues regenerating for 6-12 months. This creates a disconnect between what you see (healed incisions) and what you feel (ongoing discomfort during certain movements or positions).
Sleep quality impact: This sensitivity directly affects how well you sleep. Even mild discomfort can prevent you from entering deep, restorative sleep stages. Studies show that surgical patients who achieve comfortable sleep positioning recover faster, require less pain medication, and report better emotional wellbeing during recovery. The transition to comfortable side sleeping isn't just about position preference—it's about accessing the quality sleep your body needs for optimal healing.
Phantom Sensation and Body Image Adjustment
For patients without immediate reconstruction, side sleeping requires adjusting to dramatically different body contours. Phantom sensations can make side sleeping psychologically uncomfortable even when physically safe. Body image integration typically requires 6-12 months, and side sleeping forces you to experience your changed body in ways daytime activities don't.
These phantom sensations aren't psychological problems—they're neurological phenomena. Your brain's body map (cortical homunculus) takes time to remap after significant tissue removal. During this remapping period, you may experience sensations as if removed tissue is still present, particularly during activities like side sleeping that would have involved that tissue.
Drain Site Aftermath and Internal Healing
Even after drain removal, placement sites remain tender for weeks. Internal scar tissue creates pulling sensations when shifting positions, making side sleeping feel restrictive. This internal healing continues for 6-12 months, meaning comfort often improves gradually rather than suddenly.
Scar tissue formation is a necessary part of healing, but it creates areas of reduced flexibility and altered sensation. These internal adhesions can cause unexpected pulling or tugging sensations during position changes, even when external incisions appear fully healed.

How to Make the Transition from Back Sleeping to Side Sleeping Less Painful
Your doctor required back sleeping for initial healing—that part was medically necessary. Now you're cleared to return to side sleeping, but it can hurt. The mattress creates pressure on tender chest tissue and don't prevent you from rolling onto surgical sites during sleep.
Introducing the Side Sleeping Chest Pillow: Solving the Transition Pain Point
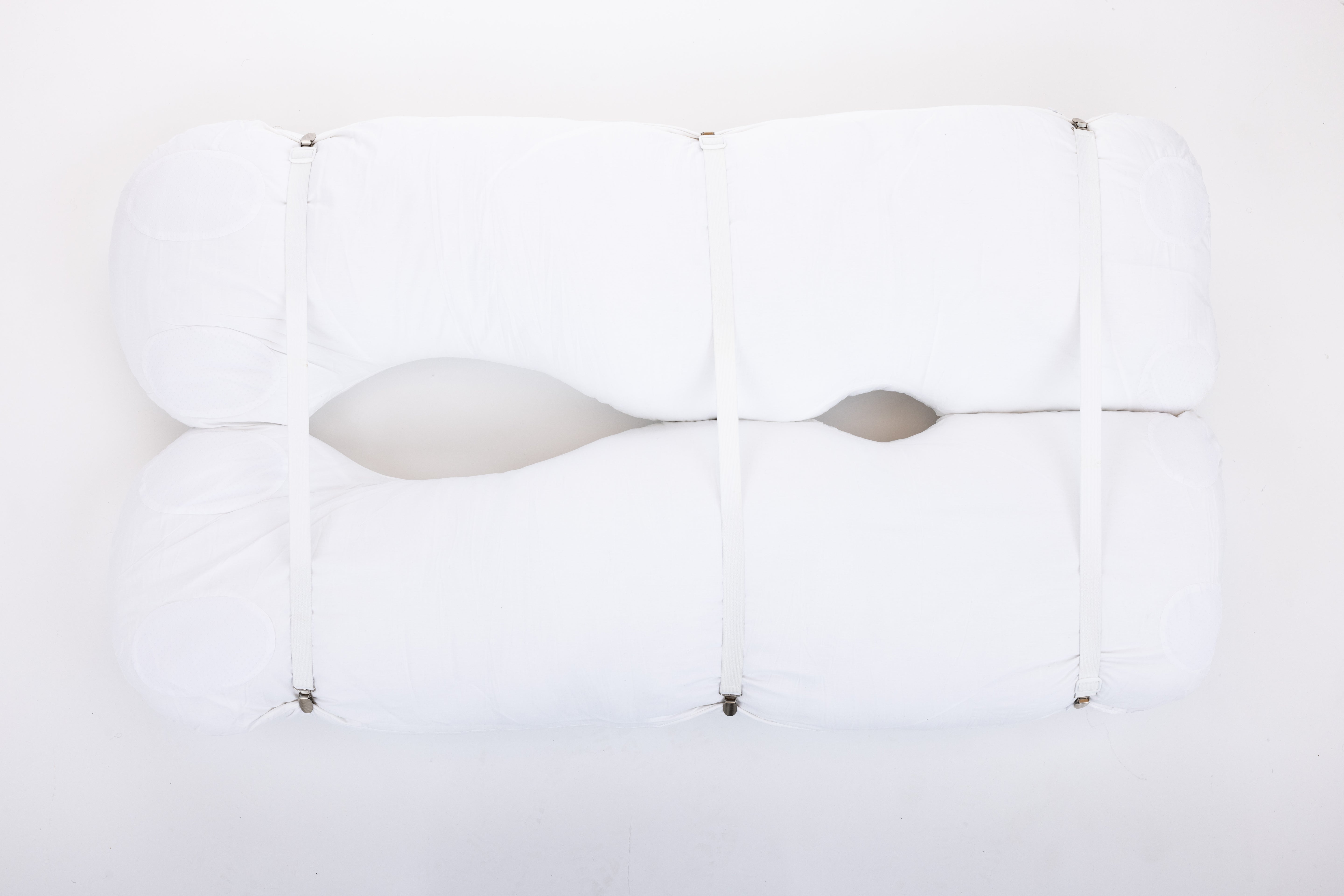
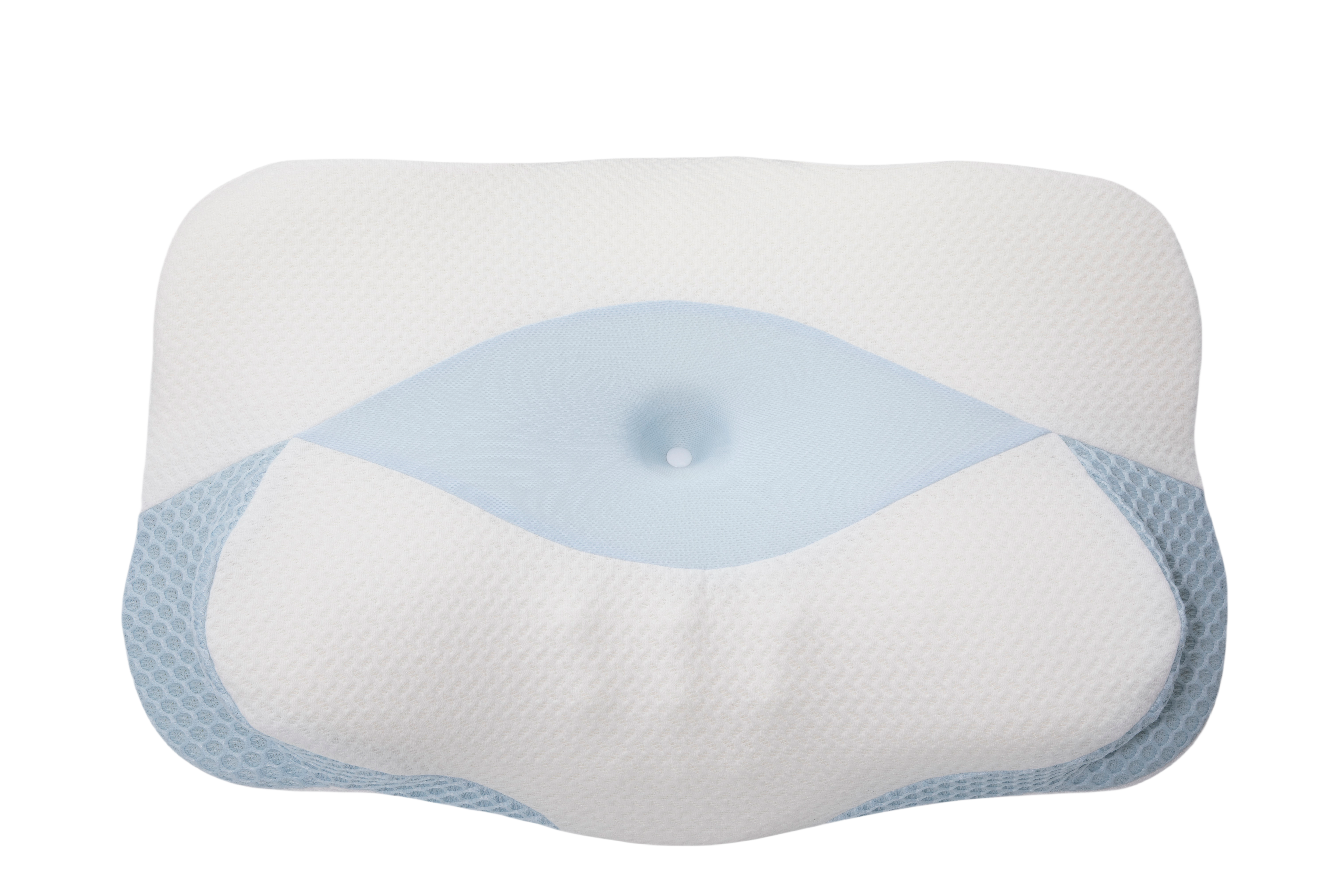
The Side Sleeping Chest Pillow was specifically created to help with the pain and discomfort of transitioning from required back sleeping to side sleeping. When doctors recommend back sleeping but you need to return to side sleeping, this pillow makes that transition actually comfortable. At $45.00 and HSA/FSA eligible, it costs less than most DIY pillow experiments.
Key features for pain-free transition:
Adjustable width: Cradles your chest without creating painful pressure on tender incisions. Configure it wider for maximum protection during those painful first weeks, or narrow it as discomfort decreases.
Symmetrical design: Turn freely to either side without losing protective support—important because you're still learning which positions hurt less during the transition.
Back support: Prevents unconscious rolling onto surgical sites during sleep, so you stay in safe positioning throughout the night.
Long-term value: Many patients continue using the pillow beyond recovery because the support quality exceeds pre-surgery sleeping arrangements.
SHOP THE SIDE SLEEPING CHEST PILLOW
Progressive Side Sleeping Strategy Using the Side Sleeping Chest Pillow
The transition period requires patience and proper support. Most patients spend 2-6 weeks gradually building confidence and comfort with side sleeping after medical clearance.
Week 1 of side sleeping clearance: Start with 20-30 minute sessions. The comprehensive support reduces anxiety about applying too much pressure while learning to trust the position again. This is the most critical week—proper support during your first attempts sets the tone for the entire transition.
Weeks 2-3: Gradually increase duration based on comfort. Most patients sleep comfortably for 2-4 hours on their side by week 2's end. The transition is progressing when you wake up on your side without pain rather than waking up because of pain.
Weeks 4-6: Many patients transition to sleeping primarily on their sides. The ability to turn freely between sides becomes increasingly valuable as recovery progresses. By this point, the transition is largely complete for most patients.
Weeks 6+: Continue using the pillow as long as it improves comfort. Many maintain use indefinitely because the support quality exceeds pre-surgery sleeping arrangements.
SHOP THE SIDE SLEEPING CHEST PILLOW
Side Sleeping Success Rates: What Makes the Difference
Understanding success rates highlights why proper support matters for your transition.
With standard sleeping arrangements:
-
First attempts (weeks 3-4): Only 40% report comfortable sleep, with most able to tolerate just 1-2 hours
-
Extended timeline (weeks 8-12): 60% achieve comfortable side sleeping, while 25% continue experiencing significant discomfort
-
Complication factors: Increased pain, frequent position changes, and anxiety about side sleeping
With purpose-designed side sleeping support:
-
First attempts: 85% report comfortable sleep within the first week
-
Extended timeline: 95% achieve comfortable side sleeping that improves overall sleep quality
-
Quality improvements: Average sleep quality scores improve 67%, daytime fatigue decreases significantly, emotional adjustment improves when physical comfort returns
Additional Strategies for Comfortable Side Sleeping
Beyond proper chest support, complementary strategies optimize your side-sleeping success during the transition period.
Compression garment coordination: Ensure garments fit without creating pressure points during side sleeping. Adjust positioning before lying down so seams don't align with incision sites. Some patients find that slightly loosening compression garments at night (with surgeon approval) reduces discomfort without compromising therapeutic benefits.
Pain management timing: Time medication to peak during intended sleep periods, helping establish comfort patterns without fighting unnecessary pain. Work with your healthcare team to develop a pain management schedule that supports your sleep goals while maintaining appropriate daytime pain control.
Room environment: Keep your bedroom cooler (65-68°F) as side sleeping generates more body heat due to increased surface contact. Use smoother sheet materials to reduce friction against compression garments. Consider moisture-wicking fabrics if night sweats are an issue during recovery.
Partner communication: Clearly communicate your needs to bed partners. Consider temporary sleeping arrangements if space constraints make comfortable side sleeping difficult. Many couples find that separate sleeping during the 4-6 week side-sleeping transition improves both partners' sleep quality without creating relationship strain.
When to Seek Medical Guidance About Side Sleeping
Certain symptoms warrant immediate consultation with your surgical team.
Contact your surgeon if you experience:
-
Increased incision pain that worsens over several days of side sleeping attempts
-
New drainage, redness, or warmth around incisions after starting side sleeping
-
Sudden arm, hand, or chest swelling developing after side sleeping
-
Sensation changes suggesting nerve compression or circulation issues
-
Visible incision changes including separation or unusual discharge
Individualized timeline variations: Your surgeon may recommend longer or shorter restrictions based on healing complications, reconstruction techniques, scar tissue patterns, or other medical conditions. Never rush clearance—there's a medical reason for their caution, and rushing risks complications requiring additional procedures.
Frequently Asked Questions About Side Sleeping After Mastectomy
Q: Can I sleep on my non-operated side immediately after a single mastectomy?
A: Most surgeons still recommend 3-4 weeks of back sleeping even for a single mastectomy before attempting any side sleeping, as even sleeping on your non-operated side creates pulling forces on your operated side.
Q: Why does side sleeping still hurt months after clearance?
A: Nerve regeneration continues for 6-12 months post-surgery, creating unpredictable sensitivity patterns. This is normal nerve recovery, not a healing problem. Proper support can significantly reduce discomfort.
Q: Will I ever be able to sleep comfortably on my stomach again?
A: Most patients can return to stomach sleeping 12-16 weeks post-surgery, though many find they need to permanently modify or avoid this position due to ongoing chest sensitivity.
Q: Can side sleeping affect my reconstruction results?
A: Side sleeping at appropriate timelines with proper support doesn't affect results. However, side sleeping too early or without adequate support can contribute to implant malposition or asymmetry issues.
Q: Can the Side Sleeping Chest Pillow be returned if it doesn't work for me?
A: Due to federal regulations, bedding products are not returnable, and all sales are final. This is why understanding your specific needs and reviewing the adjustable features is important before purchase. The pillow's adaptable design accommodates different recovery stages and body types.
Q: Is the Side Sleeping Chest Pillow covered by insurance or HSA/FSA?
A: The Side Sleeping Chest Pillow is HSA/FSA eligible, allowing you to use pre-tax dollars for your purchase. This effectively reduces the cost by 25-40%, depending on your tax bracket. Check with your HSA/FSA administrator for specific reimbursement procedures.
Making the Side Sleeping Investment: Why Proper Support Matters
The DIY reality: Patients attempting DIY solutions typically invest $60-120 in various pillows, spending 15-20 minutes nightly arranging them and waking 2-4 times for readjustments. Only 35% achieve adequate support, with 65% eventually seeking purpose-designed solutions after weeks of inadequate sleep.
The Side Sleeping Chest Pillow advantage: At $45.00, it costs less than most DIY experiments while providing purpose-designed support from first use. The adjustable design adapts to changing recovery needs, eliminating trial-and-error frustration.
HSA/FSA eligible: Use pre-tax dollars to effectively reduce the cost, making purpose-designed support more affordable than piecing together standard pillows, which aren’t HSA/FSA eligible.
Your Side Sleeping Recovery Roadmap
Understanding the progression helps set realistic expectations and reduces transition anxiety.
Phase 1 (Weeks 1-3): Exclusive elevated back sleeping. Side sleeping isn't possible—focus on optimizing back-sleeping comfort.
Phase 2 (Weeks 3-8): Continued back sleeping with gradual elevation reduction. Some single mastectomy patients may receive clearance for non-operated side sleeping during this phase.
Phase 3 (Weeks 8-12): Side sleeping clearance for most patients. The Side Sleeping Chest Pillow becomes essential for comfortable, protected side sleeping. Start with short periods and gradually increase.
Phase 4 (Weeks 12+): Most patients achieve comfortable side sleeping, approaching pre-surgery patterns. Continued support optimizes comfort and may prevent long-term positioning issues.
Long-term (6+ months): Full recovery achieved, though many maintain support habits because they improve overall sleep quality beyond recovery needs.
Taking Control of Your Side Sleeping Recovery
Your doctor required back sleeping for medical reasons. Now you're cleared for side sleeping, but it hurts to actually do it. Standard pillows weren't designed for this specific problem: supporting tender, healing chest tissue during the transition from required back sleeping to comfortable side sleeping.
Your surgeon provides the medical timeline and clearance. The Side Sleeping Chest Pillow provides the physical comfort that makes the transition from doctor-required back sleeping to side sleeping actually tolerable.
Better sleep means better healing, improved pain management, and faster return to normal activities. Having proper transition support ready when your surgeon clears you means you can return to side sleeping without weeks of painful attempts with standard pillows that don't address post-mastectomy needs.
Medical Disclaimer
This information is provided for educational purposes only and should not replace professional medical advice from your surgical team. Mastectomy procedures vary significantly in technique, extent, and individual patient factors that affect recovery timelines.
Always follow your surgeon's specific post-operative instructions regarding sleep positioning, physical activity restrictions, and recovery milestones. These medical guidelines take precedence over any general information provided here.
Contact your healthcare provider immediately if you experience signs of complications, including fever, sudden increase in pain, wound drainage, significant swelling, or breathing difficulties during recovery. Your surgical team knows your specific case and can provide guidance appropriate to your individual situation.
The mention of specific products is for informational purposes only and does not constitute medical endorsement. Consult your surgical team about positioning support options appropriate for your recovery needs. Every patient's recovery is unique, and equipment that works well for one patient may not be suitable for another based on individual medical factors.