Sciatica pain continues through the night. That radiating pain from your lower back down through your leg follows you into bed, making sleep difficult when your body needs rest most. The burning, tingling, or shooting pain that started as a daytime problem becomes worse at night when you're trying to find a comfortable position.
If you've spent the past several nights rearranging pillows and shifting positions every twenty minutes, you're not alone. The position you sleep in directly affects sciatic nerve pressure, and finding the right setup can determine whether you wake up exhausted or get the restorative rest your body needs to heal.
This guide will show you exactly how to position yourself for maximum relief, which positions worsen nerve compression, and how to create a sleep environment that supports healing rather than aggravating your condition.
Why Sciatica Disrupts Sleep
Understanding why sciatica worsens at night helps you address the causes. Your sciatic nerve runs from your lower back through your hips and down each leg. When this nerve becomes compressed or irritated, it causes the characteristic pain, numbness, and tingling that can make finding a comfortable sleep position nearly impossible.
Several factors make nighttime particularly challenging:
-
Prolonged stillness increases stiffness: When you lie in one position for extended periods, muscles and connective tissues around the sciatic nerve pathway can stiffen, increasing pressure on the nerve. This stiffness accumulates throughout the night, which is why many people experience their worst symptoms in the early morning hours.
-
Muscle relaxation changes nerve pressure: As your muscles relax during sleep, the dynamics of nerve compression can shift. For some people, this relaxation provides relief. For others, it allows structures to settle in ways that increase nerve pressure.
-
Inflammation follows daily patterns: Inflammatory markers in your body tend to be higher at night, which can increase swelling around the sciatic nerve. This natural inflammatory rhythm, combined with the reduced movement during sleep, can intensify symptoms.
-
Position limitations eliminate comfortable options: Many natural sleep positions create angles that compress the sciatic nerve or stress the lower back structures where nerve compression often originates. This means your preferred sleeping position might be directly contributing to your nighttime pain.
The Power of Elevated Back Sleeping for Sciatica Relief
Elevated back sleeping at a 30-45 degree angle provides the most comprehensive relief for most sciatica sufferers. This position addresses multiple factors that contribute to sciatic nerve compression and creates optimal conditions for reducing inflammation and promoting healing throughout the night.
How Elevation Reduces Sciatic Nerve Pressure
When you elevate your upper body at the right angle, you create several therapeutic effects that work together to reduce nerve compression:
-
Spinal decompression through gentle traction: The elevated angle creates a mild traction effect on your spine, gently increasing the space between vertebrae where sciatic nerve roots exit the spinal column. This small increase in space can significantly reduce nerve root compression that causes radiating leg pain. Even a few millimeters of additional space can make a substantial difference in nerve function and pain levels.
-
Hip flexor relief: Elevation allows your hip flexors to relax more completely than flat back sleeping. Tight hip flexors contribute to pelvic positioning problems that can increase sciatic nerve tension. When these muscles can fully relax in the elevated position, they stop pulling your pelvis into positions that stress the nerve pathway.
-
Reduced inflammatory pressure: The gentle incline improves circulation and reduces fluid pooling in your lower back and pelvis. Better circulation means inflammatory chemicals that irritate the sciatic nerve are more efficiently cleared away. This improved drainage helps reduce the swelling that contributes to nerve compression.
-
Decreased nerve stretching: The elevated position maintains your spine in a neutral curve that minimizes stretching or tension along the sciatic nerve pathway. When your spine maintains its natural curves, the nerve can rest in its optimal position without being pulled taut or compressed.
The Optimal Elevation Angle
The 30-45 degree range provides the optimal balance between therapeutic benefit and sustainable comfort for extended sleep periods. Less than 30 degrees does not provide adequate spinal decompression or hip flexor relaxation, while more than 45 degrees becomes uncomfortable for extended sleep and can cause you to slide down during the night.
Most sciatica patients find their optimal angle around 35-40 degrees. Start with 40 degrees and adjust based on your comfort and symptom response. If you experience increased lower back discomfort, reduce the angle slightly. If you are not experiencing adequate pain relief, try increasing to 45 degrees for a few nights.
These specific angles aren't arbitrary—they're the biomechanical positions that provide maximum sciatic nerve relief. The difficulty most people encounter is maintaining them consistently throughout the night. Standard household pillows compress under body weight, losing 30-50% of their height by morning.

Stop Fighting Your Pillows. Start Healing Your Sciatica.
If you've been stacking household pillows every night only to wake up at 2 AM readjusting them, you already know the problem: standard pillows weren't designed for therapeutic positioning.
The Sleep Again Pillow System was.
We created the only complete positioning system specifically for medical recovery and chronic pain relief. Our high-density foam maintains precise elevation angles throughout the night—no compression, no sliding, no frustration.
✓ Upper body elevation that stays secure all night
✓ Leg support that prevents sliding and reduces nerve tension
✓ Two contoured side pillows to cradle your back and hips
✓ Washable covers for extended use during recovery
One complete system. Consistent relief. Better sleep starting tonight.
Shop the Sleep Again Pillow System
Strategic Side Sleeping: When Back Sleeping Needs a Break
While elevated back sleeping remains optimal for most sciatica sufferers, side sleeping can provide relief when you need positional variety. Some people find side sleeping particularly helpful during the early morning hours when symptoms often intensify.
How Side Sleeping Affects the Sciatic Nerve
Side sleeping creates different biomechanical forces than back sleeping. When you lie on your side without proper support, your top leg can pull your pelvis into rotation, directly affecting sciatic nerve tension. Your spine can also curve laterally if your waist is not properly supported, creating compression on one side of the spinal column where nerve roots exit. The key to successful side sleeping with sciatica is maintaining neutral spinal alignment and pelvic positioning through strategic pillow placement.
The Side-Sleeping Setup
Choose the right side: Generally, sleeping on the side opposite your sciatica pain helps take pressure off the affected nerve. However, some people find relief sleeping on the painful side. Your body will tell you which works better—trust your symptom response over general rules.
The pillow between your knees is essential: A firm pillow between your knees prevents your top leg from pulling your pelvis out of alignment, which directly affects sciatic nerve tension. The pillow should be thick enough to keep your hips level, typically 4-6 inches of firm support. Without this support, your top knee falls toward the mattress, rotating your pelvis and potentially increasing nerve compression.
Support your affected leg: If your top leg is the painful one, ensure it is fully supported on the pillow. Your knee should rest comfortably without creating tension through your hip. The pillow should extend from your upper thigh to your ankle for complete leg support.
Maintain spinal alignment: Your spine should remain relatively straight from your head to your tailbone when viewed from behind. Use additional support pillows to fill any gaps between your waist and the mattress. This lateral support prevents your spine from sagging into a curve that can compress nerve roots.
Sleeping Positions to Avoid with Sciatica Pain
Understanding which positions to avoid is as important as knowing the beneficial ones. Some positions can significantly worsen sciatic nerve compression and prolong your recovery.
Stomach Sleeping
Stomach sleeping forces your lower back into extension, increasing pressure on the vertebral discs and nerve roots where sciatic nerve compression often originates. This position also requires turning your head to one side, creating spinal misalignment that can contribute to nerve irritation. The combination of lumbar extension and cervical rotation creates unfavorable biomechanics throughout your spine.
Flat Back Sleeping Without Support
Lying flat on your back without any knee elevation forces your legs to extend completely, which increases tension along the sciatic nerve pathway. This straight-leg position stretches the nerve, potentially worsening compression at the nerve root level. The lack of knee support also flattens your lumbar curve, which can increase disc pressure on nerve roots.
Twisted or Asymmetric Positions
Any position that twists your spine or creates asymmetry in your pelvis can worsen sciatica. This includes sleeping with one leg bent and one straight, or positions where your upper body faces a different direction than your lower body. These twisted positions can increase nerve compression and create muscle imbalances that perpetuate your symptoms.

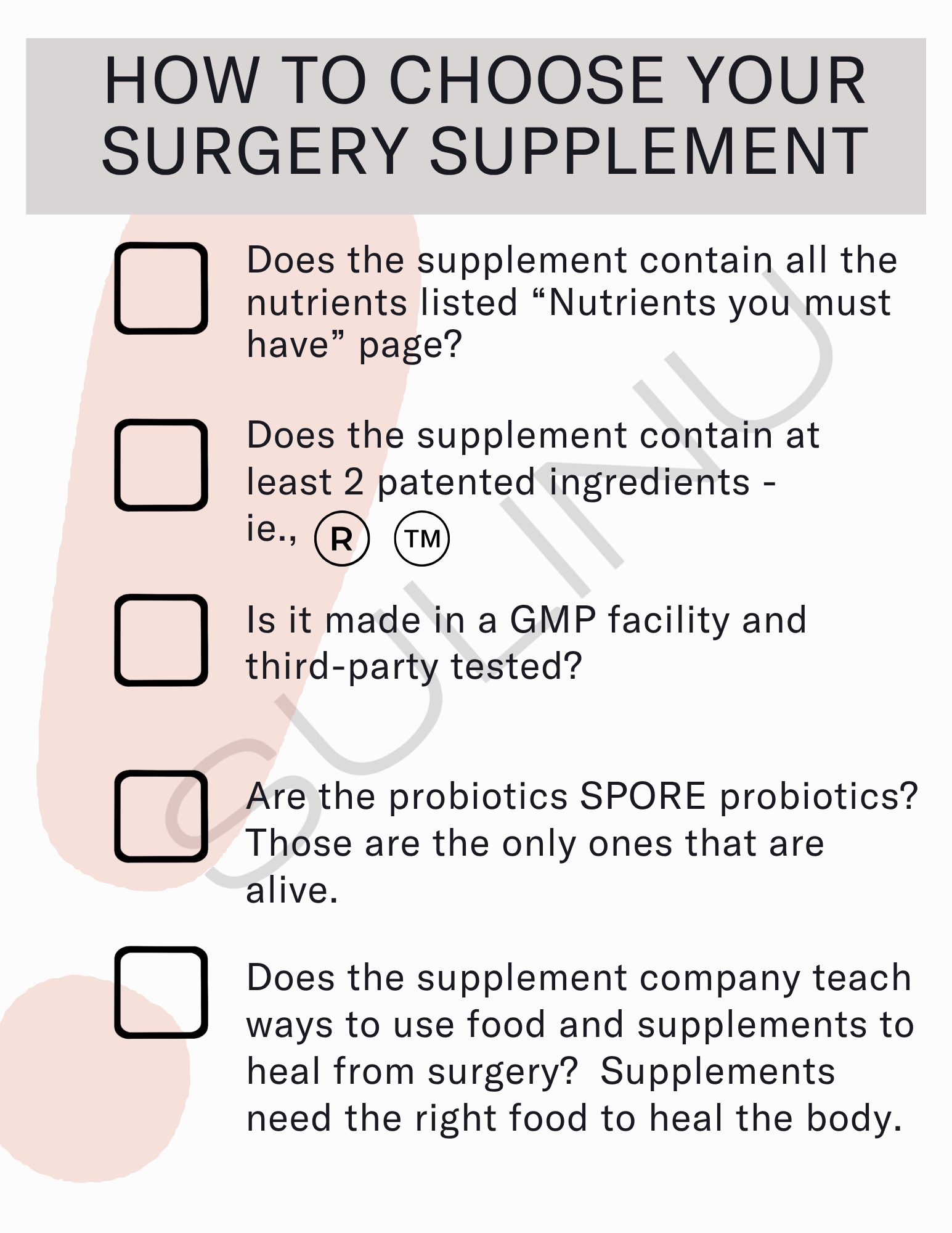
Choosing the Right Positioning Equipment
The difference between temporary relief and sustained improvement often requires having proper positioning equipment that maintains therapeutic angles throughout the entire night. Standard household pillows compress under body weight and shift during sleep, losing the therapeutic angles your body needs for healing.
Why Standard Pillows Fall Short
Regular pillows typically lose 30-50% of their height during sleep, which means the 40-degree elevation you created at bedtime might be only 20-25 degrees by morning—below the therapeutic threshold for sciatica relief. The constant compression and shifting also disrupts deep sleep phases when your body does most of its healing work. You end up waking frequently to readjust pillows, fragmenting your sleep and reducing the restorative benefits you need for nerve healing.
Professional-Grade Positioning Systems
Purpose-built positioning systems maintain therapeutic angles throughout the night without compression or shifting. These systems use high-density foam construction that provides consistent support for 8+ hours of sleep, ensuring you receive continuous therapeutic benefits rather than just the first few hours after you arrange your pillows.
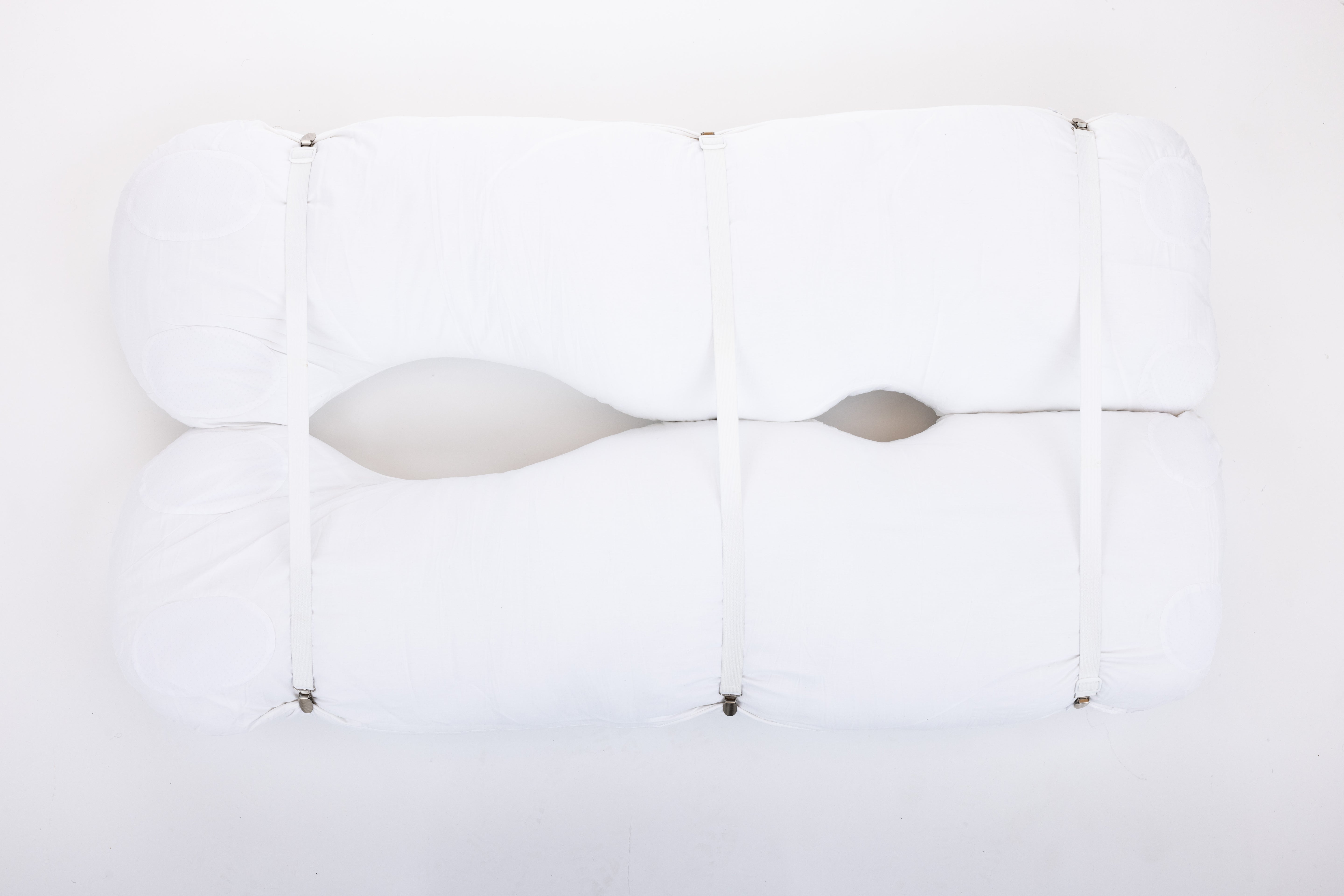
The Sleep Again Pillow System represents the most comprehensive approach to therapeutic positioning for sciatica relief. As the only full-body pillow system designed specifically for post-surgery support, chronic pain, and supporting whole body elevated sleeping, it addresses every aspect of proper positioning through integrated components that work together seamlessly.
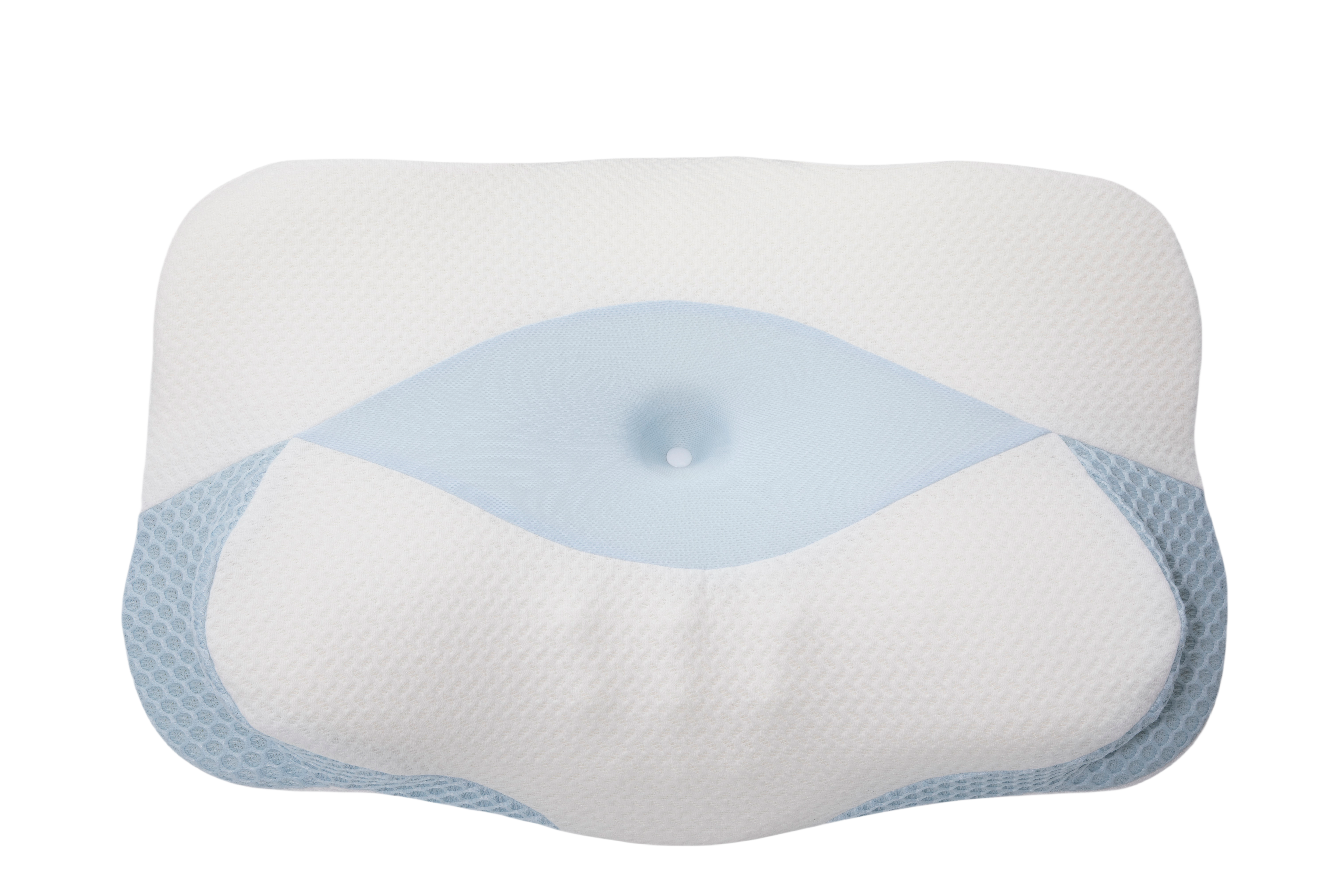
The system includes an Upper Body Wedge that maintains the precise 30-45 degree elevation for optimal spinal decompression without losing height during sleep, Contoured Side Pillows that provide the firm support needed for proper side sleeping when positional variety is desired, a Leg Support Wedge that keeps knees properly elevated to reduce sciatic nerve tension and prevent sliding, and a Head Pillow specifically designed for comfort at therapeutic elevation angles. All components feature removable, washable covers for hygiene during extended use.
The Investment in Better Sleep
Quality positioning equipment provides value beyond comfortable sleep. Proper positioning can reduce your reliance on pain medication by addressing the mechanical causes of nerve compression, improve healing through better sleep quality and reduced inflammatory cycles, prevent symptom progression by maintaining optimal nerve positioning, and provide consistent relief night after night without the frustration of pillow arrangements that fail by morning.
Many people find that investing in professional positioning equipment early prevents the trial-and-error costs of purchasing multiple inadequate pillows. The Sleep Again Pillow System's integrated design eliminates guesswork and provides proven positioning from the first night, allowing you to focus on healing rather than experimenting with pillow configurations.
Shop the Sleep Again Pillow System
Additional Strategies for Better Sleep
While positioning forms the foundation of sciatica sleep management, several additional strategies can enhance your relief and support overall healing.
Pre-Sleep Movement
Gentle movement before bed can reduce muscle tension around the sciatic nerve pathway without aggravating your symptoms. Walk for 10-15 minutes at a comfortable pace to improve circulation and reduce muscle guarding. Perform gentle hip flexor stretches to release tension that accumulates during the day. Try knee-to-chest stretches while lying on your back to gently mobilize your lower back. Always avoid aggressive stretching that increases your pain—the goal is gentle mobilization, not intensive exercise.
Temperature Management
Many people find that applying heat to the lower back and hip area 20-30 minutes before bed helps relax muscles and reduce nerve irritation. Use a heating pad on low setting or take a warm bath to promote muscle relaxation. Keep your room slightly cool (65-68°F) to support better sleep quality, but ensure your lower back and legs stay warm enough to prevent muscle tension from cold exposure.
Mattress Considerations
A medium-firm mattress typically works best for sciatica, providing enough support to maintain proper spinal alignment while offering sufficient cushioning for pressure point relief. A mattress that is too soft allows excessive spinal curvature, while one that is too firm can create pressure points that worsen discomfort. Before investing in a new mattress, try optimizing your positioning with proper support pillows—many people find that the right pillow system makes their current mattress work well.
Your Week-by-Week Progression
Week 1: Establishing Your Foundation
Focus on finding your optimal elevation angle within the 30-45 degree range. Your goal this week is establishing a position that provides noticeable relief and allows for 4-6 hour sleep stretches without significant pain interruptions. Keep a simple log of which positions work best and note any patterns in when symptoms worsen. Do not expect perfect sleep immediately—improving sleep quality is a gradual process.
Weeks 2-3: Refinement
By the second week, you should have identified positioning that provides reliable relief. Focus on maintaining consistency with your sleep setup to reinforce your body's adaptation to therapeutic positioning. Many people experience increased stiffness in the early morning hours (3-5 AM) due to natural inflammatory patterns—this is when your positioning setup becomes most critical. If morning stiffness remains problematic, consider maintaining slightly higher elevation throughout the night.
Week 4 and Beyond: Gradual Evolution
As your symptoms improve, you may gradually reduce your elevation angle or experiment with side sleeping for longer periods. Make changes slowly—reduce elevation by 5-10 degrees at a time and maintain each new position for several nights before further adjustment. This gradual approach allows your body to adapt without triggering symptom flare-ups. Some people find they prefer maintaining elevation long-term even after symptoms resolve, as the position provides ongoing benefits for spinal health.
When to Seek Medical Help
While proper sleep positioning can provide significant relief, certain symptoms indicate you need professional evaluation:
-
Progressive weakness: Increasing difficulty lifting your foot, standing on your toes, or controlling your leg movements indicates worsening nerve compression that may require medical intervention.
-
Bowel or bladder changes: Loss of bladder or bowel control can indicate cauda equina syndrome—a surgical emergency requiring immediate medical attention.
-
Numbness in the saddle area: Numbness in your groin, inner thighs, or buttocks area can signal severe nerve compression affecting critical nerve functions.
-
Bilateral symptoms: If pain, numbness, or weakness affects both legs simultaneously, this suggests more serious spinal cord involvement rather than isolated sciatic nerve compression.
-
Worsening symptoms: If your symptoms continue to worsen over 1-2 weeks despite optimal sleep positioning and other conservative measures.
FAQs: Sleep Positioning for Sciatica Pain
How long should I sleep in an elevated position for sciatica?
Most people benefit from elevated sleeping for 2-6 weeks during an acute sciatica episode. However, the duration depends on your symptom severity and healing progress. Some people with chronic sciatica find that maintaining elevation long-term helps prevent symptom recurrence. Listen to your body—if reducing elevation causes symptoms to return, continue with therapeutic positioning until your pain subsides.
Why does my sciatica pain increase at night?
Several factors can cause nighttime pain increases. Natural inflammatory patterns peak during nighttime hours, making nerve irritation more pronounced. Muscle stiffness accumulates from prolonged stillness, increasing pressure on the nerve pathway. Reduced distraction at night makes you more aware of pain signals that you might partially ignore during busy daytime activities. If pain consistently worsens at night despite proper positioning, work with a healthcare provider to address the underlying inflammation more aggressively.
How thick should the pillow between my knees be?
The pillow should be thick enough to keep your hips level when you are lying on your side—typically 4-6 inches of firm support. Your spine should be relatively straight rather than curved when viewed from behind. If your top hip drops toward your bottom hip, the pillow is too thin. If your top hip is pushed higher than your bottom hip, the pillow is too thick. The goal is neutral pelvic alignment.
What if my pillows keep flattening during the night?
Pillow compression is the most common reason therapeutic positioning fails during sleep. Standard household pillows lose 30-50% of their height under body weight, gradually reducing the therapeutic benefits you need. This is why purpose-built positioning equipment exists—to maintain consistent support throughout the night. If you are experiencing pillow compression problems, consider upgrading to professional-grade positioning systems designed specifically for therapeutic applications.
Is it worth investing in positioning pillows for sciatica?
Quality positioning equipment often provides better value than multiple cheaper alternatives that do not maintain therapeutic angles. The Sleep Again Pillow System, for example, maintains therapeutic positioning throughout the night without compression, potentially reducing your recovery time and improving your sleep quality significantly. Many people find that one quality positioning system works better than three or four cheaper pillows that require constant adjustment and replacement as they lose their shape.
Can sleeping positions prevent sciatica from coming back?
Maintaining good sleep positioning can be part of an effective sciatica prevention strategy. Many people who experience recurrent sciatica find that continuing to use therapeutic elevation or proper side-sleeping techniques helps prevent symptom recurrence. However, prevention also requires addressing other factors like core strength, flexibility, and body mechanics during daily activities. Sleep positioning works best as part of a comprehensive approach to spinal health.
Your Foundation for Sciatica Recovery
Sleep positioning is essential for creating optimal conditions for healing while you rest. Elevated back sleeping at 30-45 degrees provides the most reliable relief for most sciatica sufferers by reducing nerve compression, supporting natural spinal alignment, and promoting the circulation and reduced inflammation that healing requires.
Achieving relief requires having the right positioning support. Whether you choose carefully selected household pillows or invest in professional positioning systems like the Sleep Again Pillow System, the goal is creating sustainable, comfortable positioning that maintains therapeutic benefits throughout the night without constant readjustment.
Remember that sciatica recovery takes time, and sleep positioning is one component of comprehensive treatment. Work with your healthcare providers to address underlying causes while using proper positioning to manage symptoms and support healing. With consistent application of these positioning principles, most people experience significant improvement in both their nighttime comfort and their overall sciatica symptoms.
Medical Disclaimer
This information is provided for educational purposes only and should not replace professional medical advice. Sciatica can have multiple causes, including herniated discs, spinal stenosis, piriformis syndrome, and other conditions that may require different treatment approaches.
Always consult with your healthcare provider before making significant changes to your sleep positioning, especially if you have other health conditions or are experiencing severe symptoms. If you experience progressive weakness, loss of bowel or bladder control, or symptoms affecting both legs, seek immediate medical attention as these may indicate conditions requiring urgent treatment.
The mention of specific products or positioning strategies is for informational purposes only and does not constitute medical endorsement. What works for one person may not be appropriate for another. Always prioritize safety and follow your healthcare provider's specific recommendations for your situation.