If you have back surgery coming up or just had the procedure, here's what your surgeon probably spent about 30 seconds on: how you'll actually sleep while your spine heals. Spinal fusion, laminectomy, discectomy—whatever your procedure, post-surgical sleep positioning requires precision that your current pillow collection simply can't deliver.
The challenge? Most patients don't realize this until their first night home, exhausted and discovering that every familiar position is suddenly impossible.
Here's your advantage: you're reading this before that frustrating first night (or early enough to course-correct). While other patients are learning through trial and error—testing positions that stress their healing spine, losing sleep when they need it most, and scrambling to buy random pillows at 2 AM—you can set up the right positioning system now, before your body is recovering from major spinal surgery.
Back surgery sleep isn't just about comfort. Your spine needs specific support angles to minimize stress on surgical sites, reduce inflammation around healing tissues, and maintain proper alignment throughout 6-8 hour sleep periods. Get the positioning wrong, and you're not just uncomfortable—you're potentially compromising your surgical outcome and extending your recovery timeline.
The solution exists, and it's not complicated: precise therapeutic positioning using equipment designed for spinal surgery recovery. This means maintaining specific elevation angles that protect your surgical site, providing stable support that doesn't shift or compress overnight, and creating a sleep environment that works with your body's healing process instead of fighting against it.
Why Back Surgery Turns Sleep Into Advanced Engineering
Back surgery recovery sleep isn't just "uncomfortable"—it's a complete reconstruction of how you interact with horizontal positioning. Your spine has been surgically altered, which means the biomechanics of lying down have fundamentally changed, even if temporarily.
The spinal support equation changes completely: Your vertebrae, discs, or surrounding muscles have been modified through surgery, creating new structural requirements for comfortable positioning. What felt natural before surgery may now put stress on healing tissue or fail to provide the support your spine needs during recovery.
Movement becomes restricted: Most back surgeries come with specific movement limitations designed to protect healing structures. No twisting, no bending beyond certain angles, and often no lifting restrictions that extend to how you position yourself in bed. Suddenly, the simple act of rolling over requires conscious thought and planning.
Pain patterns shift and evolve: Post-surgical pain isn't just "back pain"—it can radiate to different areas, change intensity based on position, and respond differently to various support systems. What works for general back discomfort may be completely inadequate for post-surgical positioning needs.
Your spine's new normal requires accommodation: Even after healing, your spine may have different support requirements than before surgery. Learning to sleep with these changes isn't just about surviving recovery—it's about establishing sustainable long-term sleep habits that support your surgical investment.
The Back Surgery Sleep Position Hierarchy: From "Absolutely Not" to "Actually Works"
Position Level 1: The Forbidden Zone
Stomach sleeping: Unless you've developed the ability to sleep without rotating your spine, this position is typically off the table for months after back surgery. The spine rotation required for breathing while face-down creates exactly the kind of stress your healing back needs to avoid.
Unsupported side sleeping: While side sleeping might eventually become possible, doing it without proper support can create spine misalignment that puts pressure on healing surgical sites.
Flat back sleeping without elevation: Lying completely flat often increases pressure on the lower spine and can make getting up significantly more difficult and painful.
Position Level 2: Proceed with Caution (And Lots of Support)
Supported side sleeping: With comprehensive pillow support systems, side sleeping may become possible weeks into recovery. This requires maintaining spine alignment through strategic pillow placement and ensuring no twisting occurs during sleep.
Modified back sleeping: Some patients find success with back sleeping using leg elevation and lumbar support, though this requires careful attention to spinal alignment.
Position Level 3: Your New Recovery Headquarters
Elevated back sleeping: This becomes the foundation of back surgery recovery sleep for most patients. Picture yourself in a comfortable recliner position that happens to be your bed, angled just right to reduce spinal pressure while making movement easier.
The elevation angle works with gravity to reduce pressure on your spine while making the inevitable bathroom trips and position changes significantly easier. Most patients find 30-45 degrees optimal for the combination of comfort and spinal protection.

The Science of Spinal Support During Sleep
Understanding why certain positions help or hurt your recovery can guide your decision-making and help you communicate effectively with your healthcare team about your sleep challenges.
How Elevation Reduces Spinal Pressure
When you're lying flat, gravity works against your spine in ways that can increase pressure on healing structures. The elevated back position distributes body weight more evenly and reduces the load on your lower spine specifically.
Disc pressure reduction: If your surgery involved disc work, elevation can significantly reduce the pressure on these structures compared to flat positioning.
Muscle tension relief: Elevation allows your back muscles to relax more completely, reducing the protective muscle spasms that often develop after spinal surgery.
Improved circulation: The gentle incline assists blood flow to healing tissues while reducing pooling that can occur with flat positioning.
The Movement Mechanics Advantage
Getting in and out of bed becomes exponentially easier from an elevated position. Rather than engaging your core muscles and spine to rise from flat (exactly what you're trying to avoid), elevation lets you work with gravity instead of against it.
This movement advantage isn't just about comfort—it directly impacts your recovery success. When getting up is easier, you're more likely to move as recommended, use the bathroom when needed, and participate in prescribed activities that support healing.

Creating Your Back Surgery Sleep Support System
The foundation of successful back surgery sleep lies in creating stable, consistent support that maintains therapeutic positioning throughout the night.
Why Standard Pillows Fail for Spinal Support
Regular household pillows compress under body weight, losing the precise angles and support your healing spine requires. They shift during normal sleep movement, creating gaps in support exactly when you need it most. Most importantly, they can't maintain the consistent spinal alignment that's crucial for both comfort and healing.
The compression problem: Standard pillows lose 30-50% of their height during sleep, gradually eliminating the therapeutic positioning you carefully arranged.
The stability issue: Individual pillows move independently, creating unpredictable support that can leave your spine unsupported or misaligned during crucial healing hours.
The alignment challenge: Random pillow arrangements rarely maintain the precise spinal curves and support zones that back surgery recovery requires.
Professional-Grade Support Solutions
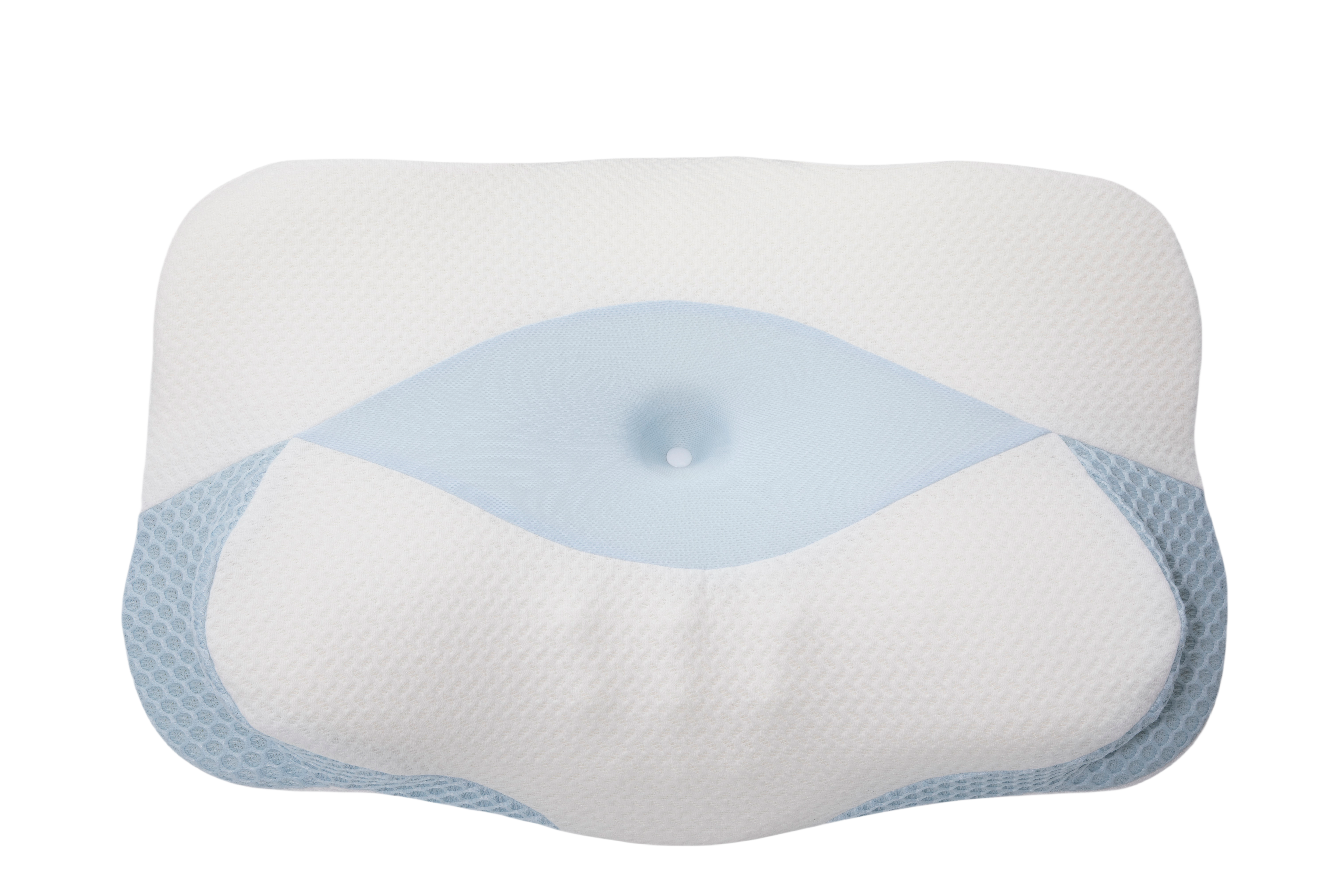
For patients who want reliable, consistent support throughout their recovery, the Sleep Again Pillow System provides comprehensive spinal support through integrated design and medical-grade materials.
Every Sleep Again Pillow System includes:
-
Two Contoured Side Pillows to cradle back and hips
-
Upper Body Wedge to create optimal upper body incline
-
Leg Support Wedge to gently elevate legs
-
Head Pillow to provide head support and neck mobility
-
Removable, washable slipcovers for every piece
SHOP THE BEST PILLOW FOR BACK SURGERY RECOVERY

Why Sleep Again Pillow System Excels for Back Surgery Recovery
Maintains spinal alignment consistently: The Sleep Again Pillow System and its components work together to maintain the precise spinal curves and support zones that back surgery patients need, unlike individual pillows that shift and compress throughout the night.
Prevents movement-related complications: The stable positioning reduces the likelihood of unconscious movements that could stress healing spinal structures, providing confidence for deeper, more restorative sleep.
Accommodates recovery equipment: The thoughtful design works with back braces, lumbar supports, and other recovery equipment rather than creating interference or pressure points.
Adapts as recovery progresses: The modular design allows adjustment as healing progresses and positioning restrictions are gradually lifted, providing value throughout the entire recovery timeline.
LEARN MORE ABOUT THE SLEEP AGAIN PILLOW SYSTEM
Week-by-Week Back Surgery Sleep Strategy
Back surgery recovery follows predictable phases, and your sleep approach should evolve to match your body's changing needs and capabilities.
Weeks 1-2: Foundation and Protection Phase
Primary position: Elevated back sleeping at 40-45 degrees with comprehensive support
Focus: Pain management, spinal protection, and establishing sustainable positioning routines
Sleep expectations: 3-5 hour stretches with wake-ups for medication and bathroom needs
During this phase, comfort takes priority over sleeping through the night. Your body is managing acute surgical stress, and fragmented sleep is normal and expected. The goal is to create consistent, safe positioning that protects your spine while allowing whatever rest is possible.
Key strategies:
-
Take pain medication 30-45 minutes before attempting sleep
-
Use the same positioning setup every night to build familiarity
-
Keep essentials within easy reach to minimize movement
-
Accept that perfect sleep isn't the goal—healing rest is
Weeks 3-4: Stabilization Phase
Primary position: Elevated back sleeping at 30-40 degrees with possible side sleeping trials
Focus: Refining positioning based on healing progress and comfort feedback
Sleep expectations: 4-6 hour stretches with improved overall comfort
As acute surgical effects subside, you can begin experimenting with position modifications and potentially introducing supported side sleeping for brief periods. This phase is about building on what worked in the first weeks while carefully expanding options.
Key strategies:
-
Test new positions during daytime rest before trying them for full night sleep
-
Maintain elevation as your primary position but explore comfort refinements
-
Begin gentle transition planning based on surgeon feedback
-
Document what works best for future reference
Weeks 5-8: Expansion Phase
Primary position: Flexible based on healing progress, often 30-degree elevation with side sleeping options
Focus: Gradually returning to more normal sleep patterns while maintaining spinal protection
Sleep expectations: 6-8 hours with improved sleep quality and fewer interruptions
This phase represents the transition from acute recovery sleep to longer-term positioning strategies. Many patients find their optimal long-term sleep setup during this period.
Key strategies:
-
Work closely with your surgical team to understand position clearances
-
Begin planning for eventual return to preferred positions
-
Consider which recovery strategies you want to maintain permanently
-
Address any persistent sleep issues with professional help
Weeks 9-12+: Integration Phase
Primary position: Based on individual healing and surgeon clearance Focus: Establishing sustainable long-term sleep habits that support spinal health Sleep expectations: Near-normal sleep duration and quality
Many patients discover that some recovery positioning strategies continue providing benefits even after medical restrictions are lifted. This phase is about integrating the most helpful aspects of your recovery sleep strategy into your permanent routine.
The Complete Sleep Environment Optimization
Successful back surgery sleep requires more than just positioning—your entire sleep environment needs to support recovery.
Temperature and Air Quality Management
Keep your room cooler than usual (65-68°F): Recovery positioning often involves more pillows and elevation that can trap body heat. Cooler temperatures help maintain comfort throughout the night.
Ensure adequate ventilation: Good air circulation becomes more important when you're spending extended time in bed and may be using additional bedding or positioning equipment.
Consider air quality: If you're sensitive to dust or allergens, recovery is a good time to address these issues since you'll be spending more time in your bedroom.
Lighting and Sound Control
Install bedside lighting that doesn't require reaching: Recovery often involves middle-of-night movement for medication or bathroom trips. Easily accessible lighting reduces the risk of injury from navigating in darkness.
Use blackout curtains or eye masks: Deep sleep becomes even more important during recovery, and controlling light exposure helps maintain natural sleep cycles that may be disrupted by medication or schedule changes.
Consider white noise or earplugs: Recovery sleep is often lighter than normal sleep, making you more sensitive to household sounds that could interrupt rest.
The Recovery Bedside Station
Essential accessibility: Keep water, medications, tissues, phone, and any medical supplies within arm's reach. The goal is minimizing movement while ensuring you have everything needed for comfort and safety.
Emergency considerations: Have a way to call for help if needed, especially during the early recovery weeks when movement is most restricted.
Comfort extras: Keep extra pillows, blankets, or positioning aids readily available for middle-of-night adjustments without major disruption.
Troubleshooting Common Back Surgery Sleep Problems
"I can't get comfortable no matter what I try."
This usually indicates that your support system isn't providing adequate spinal alignment or you're not achieving true therapeutic elevation. The solution often lies in upgrading from makeshift pillow arrangements to purpose-built positioning systems that maintain consistent support.
"I wake up with more pain than when I went to sleep."
Morning pain increases often result from poor positioning that allows your spine to settle into misalignment during sleep. Focus on maintaining consistent elevation and spinal support throughout the night rather than hoping random pillow arrangements will work.
"I'm afraid to move during sleep."
This anxiety is completely normal and actually protective during early recovery. The solution is creating positioning systems that make harmful movements difficult while providing confidence that small, necessary movements won't cause problems.
"My partner can't sleep because of all the positioning equipment."
Recovery positioning does require more bed space and equipment than normal sleep setups. Consider temporary separate sleeping arrangements or invest in space-efficient positioning systems that provide maximum support with minimal bed invasion.
Sleep Again Pillow System: Investment Analysis for Back Surgery Recovery
Most back surgery patients end up purchasing multiple rounds of pillows and support equipment before finding something that works consistently, often spending $200-300 total while dealing with weeks of inadequate support.
DIY Approach Costs:
-
Multiple pillow purchases: $150-250 across several attempts
-
Setup time: 20-30 minutes nightly arranging and testing stability
-
Sleep disruption: Multiple wake-ups for repositioning when supports collapse
-
Trial and error frustration: Weeks of poor sleep while finding what works
Sleep Again Pillow System Value:
-
Complete integrated solution: One comprehensive system designed specifically for post-surgical recovery
-
Setup time: 5 minutes once familiar with configuration
-
Consistent support: Maintains positioning throughout 8+ hours of sleep
-
Professional guidance: System comes with positioning guides specific to different surgery types
The recovery timeline consideration: Back surgery recovery typically takes 3-6 months, making the investment in quality positioning equipment economical when calculated per night of improved sleep during this crucial healing period.
GET THE HEALING REST YOU NEED FOLLOWING BACK SURGERY
Frequently Asked Questions About Back Surgery Sleep
Q: How long will I need to sleep in modified positions after back surgery?
A: Most patients need 6-12 weeks of modified positioning, though this varies significantly based on surgery type and individual healing. Fusion surgeries typically require longer positioning restrictions than discectomies. Always follow your surgeon's specific timeline.
Q: When can I return to stomach sleeping after back surgery?
A: Stomach sleeping is usually the last position cleared by surgeons, often requiring 3-6 months depending on the procedure. Some patients find they need to permanently modify or abandon this position based on their spine's new structural requirements.
Q: Is it normal to need more sleep during back surgery recovery?
A: Yes, your body requires additional energy for healing, and many patients need 1-2 more hours of sleep per night during the first month of recovery. Quality sleep becomes even more important when quantity is limited by comfort challenges.
Q: Why does my back hurt more at night after surgery?
A: Nighttime pain increases often result from accumulated daily stress on healing tissues, position-related pressure, and natural inflammatory cycles. Proper elevation and support can significantly reduce these nighttime pain spikes.
Q: Can I use a recliner instead of trying to sleep in bed?
A: Many patients find recliners comfortable during early recovery, but most sleep better in bed with proper positioning systems once established. Recliners also don't provide the bilateral support and spinal alignment that comprehensive positioning systems offer.
Q: What's the best angle for elevation after back surgery?
A: Most patients find 30-45 degrees optimal, though individual preferences vary. Start with 40-45 degrees during early recovery and gradually reduce as comfort allows. The angle should feel stable and allow easy movement for necessary activities.
Q: How do I know if my sleep position is helping or hurting my recovery?
A: Good positioning should result in consistent wake-up positions, manageable pain levels, and the ability to move when necessary without severe discomfort. If you're waking up with increased pain or stiffness, your positioning needs adjustment.
Q: Should I invest in expensive positioning equipment for temporary recovery?
A: Quality positioning systems like the Sleep Again Pillow System often provide immediate improvement and continue offering benefits long after recovery restrictions are lifted. Many patients continue using therapeutic positioning for ongoing spinal health, making it a long-term investment rather than temporary expense.
Q: What if I accidentally sleep in a restricted position?
A: Occasional brief positioning mistakes usually aren't harmful, but consistent poor positioning can interfere with healing. Use pillow barriers and positioning systems that make harmful positions difficult to achieve unconsciously.
Q: When should I contact my surgeon about sleep problems?
A: Contact your surgical team if sleep problems significantly worsen after the first week, if you experience new or severe pain with positioning changes, or if positioning issues prevent you from following other recovery recommendations.
The Bottom Line: Sleep as Spinal Medicine
Back surgery sleep challenges are complex, but they're also solvable with the right approach. The key is understanding that sleep positioning during recovery isn't just about comfort—it's a medical intervention that directly supports your surgical success.
Whether you choose carefully selected individual pillows or invest in comprehensive positioning systems like the Sleep Again Pillow System, the goal is to create sustainable support that works night after night throughout your recovery journey.
Remember that good sleep during back surgery recovery isn't a luxury—it's medicine. Your spine heals fastest when you're getting the deep, restorative sleep that only comes from proper positioning and genuine comfort. Every night of quality rest directly contributes to your long-term surgical success.
Most importantly, be patient with yourself. Back surgery recovery has its own timeline, and sleep quality often improves gradually rather than immediately. Trust the process, invest in proper support, and know that your sleep will return to normal—and may even be better than before surgery thanks to the positioning strategies you learn during recovery.
Your spine just underwent a significant investment in your long-term health and mobility. Give it the sleep support it needs to heal successfully, and both your recovery and your future self will thank you.
Medical Disclaimer
This information is provided for educational purposes only and should not replace professional medical advice. Every back surgery procedure and recovery process is unique, and sleeping position recommendations may vary significantly based on your specific surgical approach, spinal level operated on, fusion vs. non-fusion procedures, and individual health conditions.
Always follow your surgeon's specific post-operative instructions regarding sleep positioning, activity restrictions, and movement limitations. These medical guidelines take precedence over any general positioning advice provided here.
Contact your healthcare provider immediately if you experience concerning symptoms such as severe pain unrelieved by prescribed medications, numbness or tingling in your legs, difficulty with bowel or bladder function, signs of infection, or any symptoms that worsen rather than improve during recovery.