If you have a hysterectomy scheduled or just had the procedure, here's what most pre-op checklists miss: sleep positioning after major abdominal surgery requires specific planning.
Between protecting your healing incision, navigating hormonal shifts, and adapting to post-surgical restrictions, your usual sleep setup won't cut it. But here's the advantage—you can prepare the right positioning strategies now, before you're trying to problem-solve while recovering.
Most hysterectomy patients discover sleep challenges the hard way: their first night home, exhausted and sore, realizing their comfortable pre-surgery positions are suddenly impossible. Your favorite side-sleeping angle? Too much abdominal pressure. Flat on your back? Incision discomfort and potential swelling issues. Meanwhile, your body desperately needs quality rest to heal from major pelvic surgery.
The better approach? Set up your sleep success system before or immediately after surgery. This means understanding the specific positioning requirements for hysterectomy recovery, preparing the equipment that maintains therapeutic angles throughout the night, and creating an environment optimized for the healing process your body is about to undertake. When you're equipped in advance, you can focus on recovery instead of nightly trial-and-error experiments.
This isn't generic "take it easy" advice. These are targeted strategies for the unique challenges of hysterectomy recovery—from incision protection and hormonal sleep disruption to the precise elevation angles that support healing while maintaining comfort through 6-8 hour sleep periods.
Why Hysterectomy Sleep Recovery Is Unlike Any Other Surgery
Hysterectomy recovery creates a unique constellation of sleep challenges that sets it apart from other surgical recoveries. You're not just healing from an incision—you're adjusting to the removal of your uterus and potentially your ovaries, dealing with internal healing you can't see, and managing hormonal shifts that can turn your sleep patterns upside down.
Here's what makes hysterectomy recovery sleep different:
Pelvic floor disruption: Your pelvic anatomy has been fundamentally changed, affecting how you feel pressure and support throughout your core. This impacts not just comfort but also how your body naturally wants to position itself during rest.
Internal organ shifts: With your uterus removed, your other pelvic organs are literally finding new positions. This internal reorganization can create unfamiliar sensations and discomfort that affects sleep positioning in ways you never expected.
Hormonal tsunami: If your ovaries were removed, you're experiencing surgical menopause that brings immediate hot flashes, mood changes, and sleep pattern disruption. Even with ovaries intact, hormonal fluctuations from the surgery can affect your sleep quality.
Bladder sensitivity: Many hysterectomy patients experience temporary changes in bladder function, leading to more frequent nighttime trips that disrupt sleep cycles and require careful positioning to manage comfortably.
The bloating factor: Post-hysterectomy bloating isn't just uncomfortable—it's often severe enough to affect breathing and positioning comfort. This internal pressure can make lying flat feel impossible and create the need for specific positioning approaches.
Understanding Your New Sleep Geography
After a hysterectomy, your body has new rules about what feels comfortable and what doesn't. Understanding these changes helps you work with your healing body rather than fighting against it.
The Abdominal Territory Challenge
Your abdominal area now has multiple healing zones that need protection:
-
The main incision site (whether laparoscopic ports or a larger incision)
-
Internal suture lines where your cervix was separated
-
The vaginal cuff where your cervix was removed (for total hysterectomy)
-
Potential adhesion sites where tissues are healing together
Each of these areas responds differently to pressure and positioning, which is why finding comfortable sleep positions becomes so complex.
The Pelvic Pressure Points
Without your uterus providing its usual internal support structure, other organs settle into new positions. This can create:
-
Unfamiliar pressure sensations in your pelvis
-
Changes in how your back and hips feel when lying down
-
Different weight distribution that affects comfort on various surfaces
-
New sensitivity to certain sleeping angles

The Hysterectomy Sleep Position Strategy
Positions That Will Compromise Your Recovery
Flat back sleeping: While not as obviously problematic as stomach sleeping, lying completely flat often increases pressure on internal healing sites and can worsen post-surgical bloating that many hysterectomy patients experience.
Tight fetal position: Curling up in a ball puts tension on your abdominal muscles and can compress internal healing areas, potentially interfering with proper circulation to surgical sites.
Stomach sleeping: This position puts direct pressure on all your healing areas and can disrupt the internal healing process happening in your pelvic cavity.
The Hysterectomy Recovery Sweet Spot
Gentle elevated back sleeping: This becomes your recovery sanctuary. The 30-40 degree elevation specifically helps with post-hysterectomy bloating while reducing pressure on internal healing sites and making those frequent bathroom trips much easier.
Strategic side sleeping: With proper support, side sleeping can work for hysterectomy patients, but it requires specific pillow placement to support your changed pelvic anatomy and protect healing areas.
SHOP THE BEST PILLOW FOR HYSTERECTOMY
The Science Behind Elevated Sleeping for Hysterectomy Recovery
Elevated sleeping isn't just more comfortable for hysterectomy patients—it addresses the specific physiological challenges your body faces during this type of recovery.
Managing Post-Surgical Bloating
Hysterectomy patients often experience significant bloating that can last for weeks. This isn't just discomfort—it's your body's response to the manipulation of your abdominal cavity during surgery, combined with the natural healing inflammation.
The elevated position allows gravity to help distribute this bloating more evenly rather than concentrating pressure in your lower abdomen. This can provide significant relief and help you achieve more comfortable sleep positions.
Supporting Internal Healing
Your pelvic organs are reorganizing themselves after surgery, and proper positioning can support this natural process. Elevation reduces the gravitational pressure on your pelvic floor and internal healing sites, potentially reducing complications and promoting optimal healing.
Hormone-Related Sleep Benefits
If you're experiencing hot flashes and night sweats from sudden hormonal changes, the elevated position often provides better air circulation and temperature regulation compared to flat sleeping. This can help manage some of the sleep disruption caused by hormonal fluctuations.

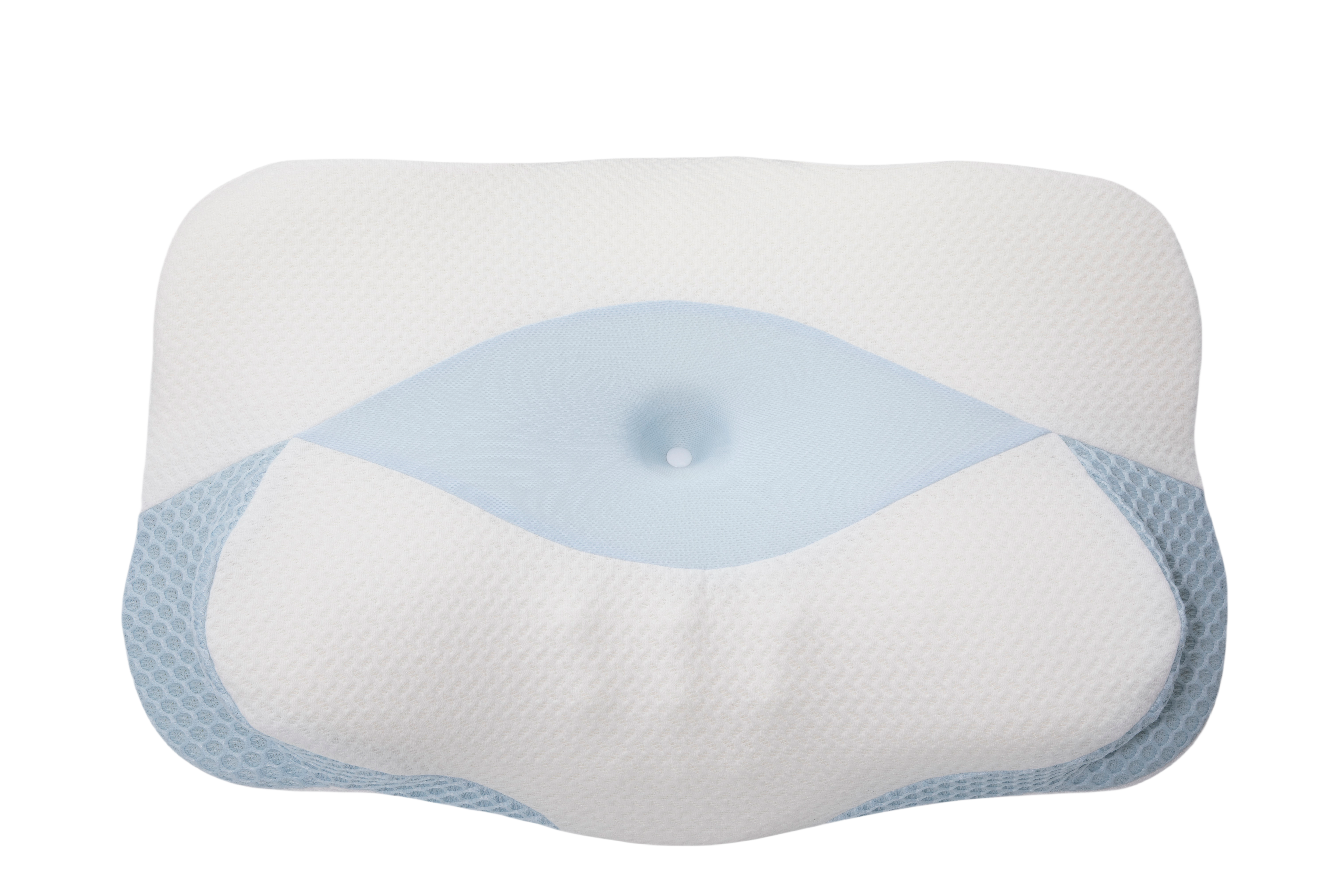
The Sleep Again Pillow System: Specialized Support for Hysterectomy Recovery
The Sleep Again Pillow System, designed specifically for post-surgical recovery, can address the comprehensive support that hysterectomy recovery requires, targeting both the immediate post-surgical needs and the ongoing comfort challenges that this type of surgery creates.
The Sleep Again Pillow System typically includes:
-
Contoured side pillows specifically shaped to support your changed pelvic anatomy
-
Upper body wedge that creates the optimal 30-40 degree elevation for hysterectomy recovery
-
Leg support components that help maintain proper positioning without straining healing abdominal muscles
-
Head pillow designed to provide comfort during extended periods of elevation
-
Removable, washable covers essential for managing post-surgical hygiene needs
SHOP THE BEST PILLOW FOR HYSTERECTOMY
 Why the Sleep Again Pillow System Excels for Hysterectomy Patients
Why the Sleep Again Pillow System Excels for Hysterectomy Patients
Addresses pelvic anatomy changes: The Sleep Again Pillow System is specifically shaped to provide support for your body's new internal geography, offering comfort that accounts for how organ positioning has changed after hysterectomy.
Maintains consistent therapeutic angles: The Sleep Again Pillow System creates the precise elevation angle that helps redistribute post-surgical bloating while supporting comfortable breathing when internal pressure makes flat positioning uncomfortable.
Accommodates recovery equipment: The Sleep Again Pillow System's stable positioning works with compression garments, support belts, or other recovery equipment without creating pressure points or comfort conflicts.
Adapts to changing needs: As your recovery progresses and your internal healing evolves, the Sleep Again Pillow System can be reconfigured to match your changing comfort requirements.
SHOP THE BEST PILLOW FOR HYSTERECTOMY
Your Recovery Sleep Timeline: What to Expect
Week 1-2: The Foundation Phase
Primary focus: Protecting all healing sites while managing acute post-surgical symptoms
This is your gentlest phase, where elevated back sleeping at 35-40 degrees becomes your default position. Your body is dealing with surgical trauma, potential gas bloating, and the beginning of hormonal adjustments.
Unique hysterectomy considerations:
-
Manage vaginal discharge by using appropriate protection that doesn't interfere with positioning
-
Be prepared for emotional responses to positional changes—many women find certain positions emotionally triggering after hysterectomy
-
Focus on positions that make frequent bathroom trips easier
Week 3-4: The Adaptation Phase
Primary focus: Beginning to expand position options while monitoring internal healing responses
You may be able to reduce elevation slightly (30-35 degrees) and experiment with supported side sleeping if comfortable. This is when many women start to feel their internal anatomy "settling" into new patterns.
Hormone management integration: If experiencing surgical menopause symptoms, this is when sleep positioning strategies need to accommodate hot flashes and temperature regulation needs.
Week 5-8: The Integration Phase
Primary focus: Gradually returning to varied positions while respecting ongoing healing needs
Your external incisions may be well-healed, but internal healing continues. You can often sleep at gentler angles and may begin longer periods in side positions, but listen carefully to your body's responses.
Beyond Week 8: The New Normal Phase
Primary focus: Establishing sustainable long-term sleep patterns that work with your body's permanent changes
Many hysterectomy patients discover that some of the positioning strategies they learned during recovery continue to provide benefits. Your pelvic anatomy has permanently changed, and your optimal sleep positions may be different than before surgery.
Managing Complex Hysterectomy Sleep Challenges
Surgical Menopause Sleep Disruption
If your hysterectomy included ovary removal, you're dealing with immediate surgical menopause that can severely disrupt sleep patterns beyond just positioning challenges.
Temperature management strategies:
-
Keep your bedroom between 65-68°F and use moisture-wicking bedding materials
-
Choose breathable materials for positioning pillows to prevent heat retention
-
Use layered, easily adjustable bedding that can be modified as your temperature fluctuates
-
Position fans to promote air circulation around your elevated sleeping position
Sleep pattern stabilization:
-
Maintain consistent bedtime and wake-up times even when sleep quality fluctuates
-
Use blackout curtains and minimize blue light exposure in the evening
-
Consider discussing hormone replacement therapy options with your healthcare provider
Emotional Sleep Challenges
Hysterectomy recovery often includes emotional adjustments that can affect sleep quality in ways that other surgeries don't typically involve.
Position associations: Some women find that certain sleep positions trigger emotional responses related to their surgery or changes in their body. Be patient with these responses and modify positions as needed for emotional comfort.
Identity adjustment: The removal of reproductive organs can trigger complex feelings about femininity, aging, and identity that may surface during quiet sleep time. Consider counseling support if these feelings significantly impact sleep quality.
Partner considerations: Changes in physical intimacy comfort levels may affect sleep positioning preferences and bed sharing arrangements. Open communication about temporary needs can help maintain relationship support during recovery.
Persistent Bladder Changes
Strategic positioning becomes crucial when bladder function changes create frequent sleep disruptions.
Elevation advantages: Raised positioning makes getting up and down significantly easier than flat sleeping, reducing the physical effort required for frequent bathroom trips and helping you return to sleep faster.
Bedside preparation: Keep nighttime supplies organized and easily accessible—appropriate protection, tissues, and a small flashlight—to minimize disruption during frequent trips.
Fluid timing optimization: Work with your healthcare provider to balance adequate hydration for healing with strategic timing that minimizes nighttime disruptions.
Troubleshooting Specific Hysterectomy Sleep Problems
Problem: "The internal pressure and bloating make every position uncomfortable."
Why this happens: Post-hysterectomy bloating can be severe and persistent, creating internal pressure that affects positioning comfort in unique ways.
The solution: Focus on elevation angles between 30-40 degrees that accommodate abdominal distension without compression. Avoid tight-fitting sleepwear or positioning that puts pressure on your abdomen. Consider sleeping in loose, breathable clothing that moves with your body. The Sleep Again Pillow System and its contoured design specifically accommodates post-surgical bloating without creating additional pressure points.
Problem: "I can't tell if my pain is normal or if my positioning is wrong."
Why this happens: Internal healing creates sensations that are different from typical surgical pain, making it difficult to distinguish between normal healing discomfort and positioning-related problems.
The solution: Track your pain patterns in relation to different positions. Normal healing discomfort should gradually improve over time, while positioning-related pain typically worsens with certain positions and improves with adjustment. Contact your healthcare provider if pain increases or doesn't follow expected improvement patterns.
Problem: "My pillow arrangement keeps collapsing during the night."
Why this happens: Regular household pillows compress under body weight and shift during normal sleep movement, losing the therapeutic positioning crucial for recovery.
The solution: Use firmer pillows as your foundation, add non-slip materials underneath your arrangement, and test stability before settling in for sleep. Push against your pillow setup—it should provide firm resistance without shifting. For consistent results, the Sleep Again Pillow System maintains its therapeutic positioning throughout the night, eliminating the frustration of collapsed arrangements.
Problem: "I'm exhausted, but my hormones won't let me sleep."
Why this happens: Sudden hormonal changes from surgical menopause can create intense sleep disruption that positioning alone cannot address.
The solution: Combine positioning strategies with comprehensive menopause management. Keep your bedroom cool, use breathable bedding, maintain consistent sleep schedules, and discuss medical management options with your healthcare provider.
Environmental Optimization for Hysterectomy Recovery
Creating Your Recovery Sleep Environment
Temperature control: Maintain bedroom temperature between 65-68°F, especially crucial if experiencing hormonal hot flashes. Good ventilation and air circulation around your elevated position help manage temperature fluctuations. Professional positioning systems like the Sleep Again Pillow System promote better airflow than bulky DIY arrangements.
Accessibility planning: Keep essentials within easy reach—water, medications, tissues, appropriate protection for discharge, and phone for healthcare contact if needed. Install motion-activated nightlights for safe navigation during frequent bathroom trips.
Comfort materials: Choose moisture-wicking sheets and lightweight blankets that can be easily adjusted. Avoid materials that retain heat or create uncomfortable friction against healing skin. When selecting positioning equipment, prioritize breathable materials and washable covers for hygiene management.
Sound management: Use white noise machines or earplugs to mask household sounds that might disturb lighter post-surgical sleep patterns.
Space optimization: Arrange your bedroom to accommodate positioning equipment without creating clutter. The Sleep Again Pillow System and its streamlined design take up less space than equivalent DIY arrangements while providing superior support.
When to Contact Your Healthcare Team
Understanding when sleep problems require medical attention versus positioning adjustment can prevent complications and ensure optimal recovery.
Immediate medical attention needed for:
-
Signs of infection around incision sites (increased redness, warmth, swelling, or discharge)
-
Heavy bleeding or concerning changes in discharge patterns
-
Severe pain that doesn't respond to prescribed medications and positioning changes
-
Difficulty breathing or chest pain
-
Sudden, severe abdominal pain
Follow-up discussions for:
-
Sleep problems that worsen rather than improve after the first week
-
Persistent discomfort that prevents any comfortable positioning
-
Questions about when to advance to different sleep positions
-
Hormonal symptoms severely disrupting sleep quality
-
Emotional responses to surgery that significantly impact sleep
Frequently Asked Questions About Hysterectomy Sleep Recovery
Q: How does hysterectomy sleep recovery differ from other abdominal surgeries?
A: Hysterectomy involves both external healing and internal organ repositioning, plus potential hormonal changes that other abdominal surgeries don't include. This creates unique positioning needs and longer-term comfort considerations.
Q: Will I ever be able to sleep on my stomach again after a hysterectomy?
A: Most women can eventually return to stomach sleeping, typically after 8-12 weeks, but many find their comfort preferences have changed. Internal anatomy changes may make stomach sleeping less comfortable permanently.
Q: Why does the bloating last so long after a hysterectomy?
A: Post-hysterectomy bloating can persist for weeks or even months as your internal anatomy adjusts to the changes. Proper positioning can help manage this discomfort while healing progresses.
Q: How long will I need modified sleep positions?
A: Most women need 6-8 weeks of modified positioning, but internal healing and hormonal adjustments may create ongoing comfort preferences that differ from pre-surgery patterns.
Q: Can sleep problems affect my hysterectomy recovery?
A: Yes, poor sleep can slow healing, worsen pain perception, and interfere with emotional adjustment to surgery. Prioritizing sleep quality supports optimal recovery outcomes.
Q: Should I be concerned about sleeping alone during recovery?
A: Many women sleep alone during hysterectomy recovery without problems. Ensure you have easy access to communication tools and emergency contacts, and discuss any specific concerns with your healthcare provider.
Q: How do I know if my sleep position is helping or hurting my recovery?
A: Helpful positioning should result in gradually improving comfort over time, stable pain levels or improvement, and the ability to sleep for longer periods. Worsening pain, increased swelling, or new discomfort may indicate positioning problems.
Long-Term Sleep Success After Hysterectomy
Unlike many surgical recoveries where you simply return to previous patterns, a hysterectomy often results in discovering new sleep preferences that work better with your body's permanent changes.
Ongoing Benefits of Recovery Positioning
Many women find that positioning strategies learned during recovery provide lasting improvements:
-
Better temperature regulation for ongoing menopausal symptoms
-
Improved comfort accommodating changed pelvic anatomy
-
Easier nighttime mobility for continuing bladder sensitivity
-
Enhanced overall sleep quality from optimized body alignment
Making Equipment Decisions
The Sleep Again Pillow System often provides value extending well beyond recovery, as the anatomical changes from hysterectomy may create permanent benefits from elevated sleeping and comprehensive body support.
Consider your long-term sleep goals when evaluating equipment investments. What begins as recovery necessity often becomes lasting sleep quality improvement.
The Bottom Line: Your Hysterectomy Recovery Sleep Success
Hysterectomy recovery sleep requires understanding and working with your body's unique changes rather than fighting against them. The combination of internal healing, potential hormonal shifts, and anatomical modifications creates challenges that generic post-surgical advice cannot adequately address.
Success comes from recognizing that your sleep needs may be permanently different after hysterectomy, and that's completely normal. The positioning strategies that support your recovery often become lasting improvements to sleep quality and overall comfort.
Whether you choose DIY solutions or the Sleep Again Pillow System, the goal is creating sustainable comfort that supports both immediate healing and long-term wellness. Your body has undergone significant changes that deserve thoughtful, comprehensive support during this crucial recovery period.
Most importantly, be patient with yourself as you navigate not just physical healing but also potential emotional and hormonal adjustments. Your sleep patterns may take time to stabilize, but with the right approach and adequate support, you can achieve quality rest that supports optimal recovery and long-term health.
The investment in proper positioning during hysterectomy recovery—whether through carefully arranged household items or the Sleep Again Pillow System—pays dividends in faster healing, better comfort, and often improved long-term sleep quality. Your future self will thank you for prioritizing quality rest during this important transition.
Medical Disclaimer
This information is provided for educational purposes only and should not replace professional medical advice. Every hysterectomy procedure and recovery process is unique, and recommendations may vary based on your specific surgical approach (abdominal, vaginal, or laparoscopic), whether ovaries were removed, individual health conditions, and post-operative circumstances.
Always follow your surgeon's specific post-operative instructions regarding sleep positioning, activity restrictions, and recovery protocols. These medical guidelines take precedence over any general advice provided here.
Contact your healthcare provider immediately if you experience concerning symptoms such as signs of infection, heavy bleeding, severe pain unrelieved by prescribed medications, difficulty breathing, or symptoms related to potential complications.
The mention of specific products or strategies is for informational purposes only and does not constitute medical endorsement. Recovery needs vary significantly among hysterectomy patients based on surgery type, age, overall health, and individual healing responses.
Recovery timelines are estimates—your individual healing may differ based on factors including surgical technique, whether ovaries were removed, your overall health status, and adherence to post-operative care instructions.