If you have surgery coming up or just had a procedure, here's something your surgical team probably didn't emphasize: your sleep is about to face serious challenges. Post-surgical insomnia affects the majority of patients, yet most people walk into recovery completely unprepared for it. The good news? You now have a critical window to set up the sleep strategies that will protect your recovery before exhaustion sets in.
Here's what many people don't realize until they're in recovery: surgery doesn't just impact the surgical site. The combination of anesthesia, pain medications, disrupted circadian rhythms, physical discomfort, and your body's stress response creates a perfect storm for sleep difficulties. By the time most patients recognize they're dealing with serious insomnia, they're already exhausted and struggling to implement solutions.
The good news is that post-surgical sleep disruption, while extremely common, is both predictable and manageable. The patterns are well-documented, the contributing factors are understood, and specific evidence-based strategies can protect your sleep quality throughout recovery. More importantly, preparing these strategies before surgery—or immediately after—is far more effective than waiting until sleep deprivation compounds your recovery challenges.
This isn't about accepting poor sleep as an inevitable part of recovery. It's about recognizing that your body will be working harder than ever to heal, and that healing process fundamentally depends on reaching deep, restorative sleep phases. Setting up the right sleep environment, positioning strategies, and management techniques now means you'll have them in place exactly when your body needs them most.
The Perfect Storm: Why Surgery Turns Sleep Into Mission Impossible
Surgery creates a perfect storm of sleep-disrupting factors that would challenge even the most dedicated sleeper. Understanding why your sleep has gone haywire is the first step toward fixing it.
Your Body's Chemical Rebellion
Anesthesia hangover: General anesthesia doesn't just knock you out during surgery—it can disrupt your natural sleep-wake cycles for days or even weeks afterward. Your brain's internal clock gets confused, leading to difficulties falling asleep, staying asleep, or feeling rested when you do sleep.
Medication mayhem: Pain medications, antibiotics, and other post-surgical drugs can interfere with normal sleep patterns. Opioid pain relievers, while necessary for managing surgical pain, are notorious for disrupting REM sleep and creating fragmented sleep patterns.
Hormonal chaos: Surgery triggers a massive stress response in your body, flooding your system with cortisol and adrenaline. These stress hormones are designed to keep you alert and ready for action—exactly the opposite of what you need for quality sleep.
Physical Comfort Challenges
The positioning puzzle: Many surgeries require specific sleeping positions or restrictions that eliminate your comfortable sleep positions. Suddenly, your go-to side sleeping isn't allowed, your favorite stomach position is off-limits, and you're trying to sleep in positions that feel foreign and uncomfortable.
Pain interference: Even with medication, surgical pain can make it difficult to find comfortable positions or stay asleep when pain breaks through. The fear of accidentally moving in ways that could worsen pain keeps many patients in a state of hypervigilance that prevents deep sleep.
Equipment obstacles: Surgical drains, compression garments, slings, or other medical equipment can make normal sleep positioning impossible and create physical barriers to comfortable rest.
Mental and Emotional Factors
Anxiety and worry: Concerns about healing, recovery progress, or potential complications can keep your mind racing when it should be winding down for sleep.
Environmental disruption: Hospital stays disrupt your normal sleep environment and routine. Even after returning home, your bedroom may need modifications for recovery that change the familiar sleep cues your brain relies on.
Fear of unconscious movement: Many patients develop anxiety about moving during sleep in ways that could compromise their recovery, leading to light, restless sleep rather than the deep rest they need.
The Hidden Cost of Post-Surgical Sleep Loss
Poor sleep after surgery isn't just uncomfortable—it directly impacts your recovery in measurable ways.
Healing Consequences
Delayed wound healing: Your body's repair mechanisms are severely compromised without adequate rest, leading to slower recovery at surgical sites.
Weakened immune function: Sleep deprivation suppresses immune system function, increasing your risk of infections and other complications.
Increased inflammation: Poor sleep elevates inflammatory markers in your body, potentially prolonging swelling and discomfort at surgical sites.
Recovery Timeline Impact
Extended pain duration: Patients with poor sleep often experience more intense and longer-lasting post-surgical pain.
Slower functional recovery: Sleep deprivation affects coordination, balance, and cognitive function, potentially slowing your return to normal activities.
Mood and motivation effects: Chronic sleep loss can lead to depression, anxiety, and reduced motivation to participate in recovery activities like physical therapy.

The Sleep Architecture Solution: Building Better Post-Surgical Rest
Quality sleep after surgery requires intentional architecture—creating the physical and environmental conditions that support restorative rest despite the challenges recovery presents.
Strategic Positioning for Sleep Success
The foundation of post-surgical sleep success often lies in finding positioning that serves dual purposes: protecting your healing body while providing genuine comfort for extended rest.
Elevated back sleeping emerges as the optimal position for most surgical recoveries. This positioning reduces swelling, improves breathing, minimizes pressure on surgical sites, and makes it easier to get up for necessary movement. The therapeutic angle of 30-45 degrees provides maximum benefit while remaining comfortable for extended rest.
Supported side sleeping may be possible depending on your surgery type, but requires comprehensive pillow support to prevent rolling onto restricted areas and maintain proper alignment.
The positioning principle: Your sleep setup should make the right positions comfortable and the wrong positions difficult, removing the need to consciously monitor your position throughout the night.
The Equipment Reality Check
Standard household pillows fail during recovery because they compress under body weight, shift during sleep, and lose their therapeutic positioning when you need support most. Professional-grade positioning systems maintain consistent support throughout the night, eliminating disruptions that fragment healing rest.
 The Complete Solution for Insomnia After Surgery: Full-Body Sleep Support
The Complete Solution for Insomnia After Surgery: Full-Body Sleep Support
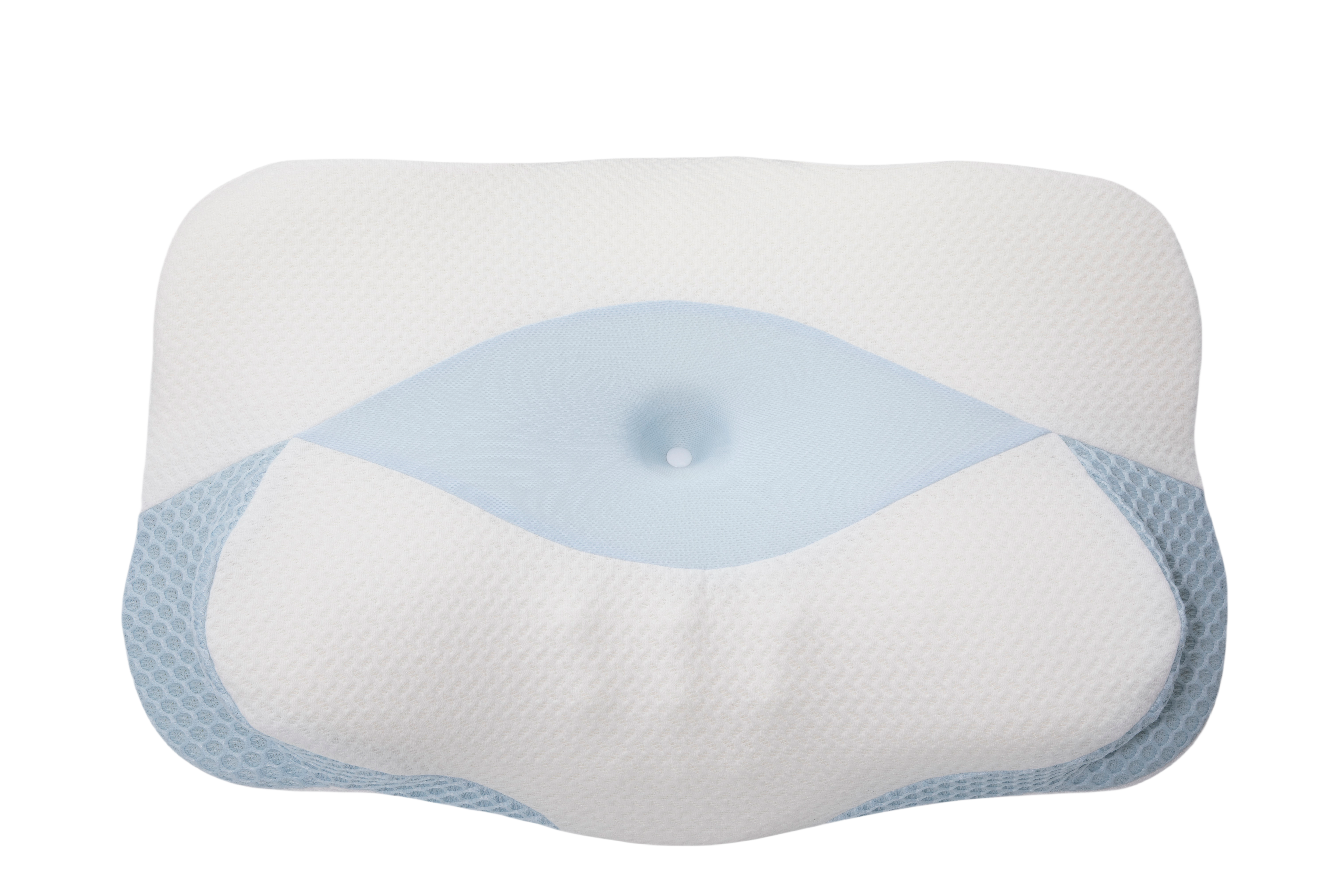
For patients seeking comprehensive solutions to post-surgical sleep challenges, the Sleep Again Pillow System addresses every positioning need through integrated design and medical-grade materials.
Every Sleep Again Pillow System includes:
-
Two Contoured Side Pillows to cradle back and hips
-
Upper Body Wedge to create optimal upper body incline
-
Leg Support Wedge to gently elevate legs
-
Head Pillow to provide head support and neck mobility
-
Removable, washable slipcovers for every piece
Why Sleep Again Pillow System Excels for Post-Surgical Insomnia
Consistent positioning throughout the night: The Sleep Again Pillow System maintains the therapeutic angles that standard pillows cannot match, eliminating positioning disruptions that commonly fragment post-surgical sleep.
Comprehensive comfort creation: Each component works with the others to create full-body support that addresses the multiple comfort challenges surgery creates.
Adaptable configuration: The modular design allows adjustment as recovery progresses and positioning needs change, providing value throughout your entire healing journey.
Sleep cycle protection: By maintaining stable positioning, the Sleep Again Pillow System reduces the physical disruptions that prevent patients from reaching the deep sleep phases crucial for healing.
SHOP THE BEST PILLOW FOR INSOMNIA AFTER SURGERY

Week-by-Week Sleep Recovery Strategy
Post-surgical insomnia follows predictable patterns, and your approach should evolve as your recovery progresses.
Week 1: Survival and Foundation Building
Primary focus: Establishing basic comfort and managing acute pain interference with sleep. Fragmented sleep with 2-4 hour stretches is normal and temporary.
Key strategies:
-
Optimal pain medication timing (take medications 30-45 minutes before bedtime)
-
Consistent positioning setup using the therapeutic elevation principles
-
Environmental comfort optimization
-
Acceptance that perfect sleep isn't the goal—healing rest is
Weeks 2-3: Pattern Establishment
Primary focus: Developing sustainable routines and refining what worked in week 1. Expect longer sleep stretches (4-6 hours) with fewer awakening episodes.
Key strategies:
-
Position refinement based on experience
-
Gradual reduction in sleep medications if possible
-
Establishment of consistent bedtime routines
-
Address medication withdrawal effects as they arise
Weeks 4-6: Normalization Phase
Primary focus: Transitioning toward normal sleep patterns while maintaining recovery support. Near-normal sleep duration with improved quality becomes achievable.
Key strategies:
-
Gradual position modifications as healing allows
-
Sleep hygiene optimization
-
Address any persistent issues with your healthcare team
-
Patience with the recovery timeline
When to Seek Additional Help
Red Flag Symptoms
Persistent insomnia beyond 2-3 weeks: If sleep problems aren't improving as your physical recovery progresses.
Sleep-related breathing issues: Snoring, sleep apnea, or difficulty breathing when lying down.
Mood changes: Significant depression, anxiety, or mood swings that may indicate sleep deprivation effects.
Cognitive impacts: Memory problems, concentration difficulties, or confusion beyond what's expected from medication effects.
Professional Support Options
Sleep specialists: Can evaluate and treat complex sleep disorders that may emerge or worsen after surgery.
Pain management specialists: May help optimize pain control strategies that support better sleep.
Physical therapists: Can assist with positioning strategies and mobility improvements that enhance sleep quality.
Mental health professionals: Can address anxiety, depression, or trauma-related sleep issues that sometimes develop after surgery.

Frequently Asked Questions About Post-Surgical Insomnia
Q: How long does insomnia typically last after surgery?
A: Most patients see significant improvement in sleep quality within 2-4 weeks after surgery. However, the timeline varies based on surgery type, individual healing rates, and how well positioning and comfort issues are addressed. Major surgeries or those requiring extended position restrictions may take 6-8 weeks for normal sleep patterns to return.
Q: Is it normal to have vivid dreams or nightmares after surgery?
A: Yes, this is very common. Anesthesia, pain medications, and the stress of surgery can all contribute to unusual dream patterns. These typically normalize as medications are reduced and your body recovers from the surgical stress response.
Q: Why do I feel tired all day but can't sleep at night?
A: This paradox often results from disrupted circadian rhythms caused by anesthesia, medications, or changed daily routines. Your sleep-wake cycle needs time to recalibrate. Maintaining consistent bedtime routines and optimizing your sleep environment can help reset these patterns.
Q: Can pain medication cause insomnia even though it makes me drowsy?
A: Absolutely. Many pain medications cause initial drowsiness but then disrupt natural sleep architecture, leading to fragmented, non-restorative sleep. This is why proper positioning and comfort measures are so important—they can help you need less medication while achieving better sleep quality.
Q: Should I nap during the day if I'm not sleeping well at night?
A: Short naps (20-30 minutes) in the early afternoon can be beneficial during recovery. However, long naps or napping late in the day can worsen nighttime insomnia. If you must nap, do so before 3 PM and keep it brief.
Q: How do I know if my sleep position is helping or hurting my recovery?
A: Good positioning should result in waking up in approximately the same position you fell asleep in, with manageable pain levels and without increased swelling. If you're consistently waking up with new aches, increased surgical site discomfort, or signs of poor circulation (numbness, tingling), your positioning needs adjustment.
Q: When can I return to my normal sleep positions?
A: This depends entirely on your specific surgery and healing progress. Always follow your surgeon's specific guidelines. Generally, minor surgeries may allow position flexibility within 2-3 weeks, while major procedures may require 6-12 weeks of modified positioning.
Q: Will my sleep patterns ever return to normal?
A: Yes, for the vast majority of patients, sleep patterns return to normal or even better than before surgery once healing is complete. Some patients discover that the positioning strategies they learned during recovery continue to benefit their sleep quality long-term.
Q: What's the difference between post-surgical fatigue and insomnia?
A: Post-surgical fatigue is feeling tired and low on energy due to the healing process—your body is working hard to repair itself. Insomnia is the inability to fall asleep or stay asleep despite being tired. You can experience both simultaneously, which is why addressing sleep quality is so important for recovery.
Q: Are expensive positioning pillows really worth it for temporary recovery?
A: Quality positioning systems often pay for themselves within the first week through improved sleep quality. Better sleep directly impacts healing speed, pain levels, and overall recovery experience. Many patients also continue using positioning systems after recovery for ongoing sleep benefits, making them a long-term investment in sleep health.
Q: How does poor sleep actually affect healing?
A: Sleep is when your body does most of its repair work. During deep sleep phases, your body releases growth hormone essential for tissue repair, consolidates immune function, and reduces inflammatory markers. Poor sleep can measurably slow wound healing, increase infection risk, and prolong recovery timelines.
Q: What should I do if I wake up in the middle of the night and can't get back to sleep?
A: Avoid looking at bright screens or clocks. Try gentle relaxation techniques like deep breathing or progressive muscle relaxation. If you're not asleep within 20-30 minutes, it's okay to get up briefly for a quiet, non-stimulating activity like reading until you feel drowsy again, then return to your proper positioning.
The Science Behind Sleep and Healing
Understanding why sleep is so crucial for recovery can motivate you to prioritize sleep strategies even when they require effort or investment.
Growth Hormone and Tissue Repair
The overnight healing factory: Your body releases the majority of growth hormone during deep sleep phases, particularly in the first few hours after falling asleep. This hormone is directly responsible for repairing damaged tissue, building new cells, and strengthening healing surgical sites.
Sleep debt consequences: When you don't reach these deep sleep phases due to positioning discomfort or fragmented sleep, you're literally missing out on your body's primary healing mechanism. This is why consistent, comfortable positioning throughout the night becomes so crucial for recovery success.
Immune System Restoration
Infection resistance: Quality sleep supports white blood cell production and function, your body's primary defense against post-surgical infections.
Inflammation management: Sleep helps regulate inflammatory responses, reducing excessive swelling while maintaining the beneficial inflammation necessary for healing.
Pain Processing and Management
Pain threshold effects: Sleep deprivation lowers your pain threshold, making the same level of discomfort feel more intense.
Endorphin production: Adequate sleep supports natural pain-relieving endorphin production, potentially reducing your need for pain medication.
Sleep as Medicine
Post-surgical insomnia is frustrating, but it's not permanent. With the right combination of positioning support, environmental optimization, and medical coordination, you can achieve the quality sleep your body needs to heal effectively.
The key is understanding that sleep during recovery isn't the same as normal sleep—it requires intentional support, proper equipment, and often temporary modifications to your usual routines. Whether you choose carefully selected individual pillows or invest in comprehensive positioning systems like the Sleep Again Pillow System, the goal is to create sustainable comfort that works night after night.
Remember that good sleep during recovery isn't a luxury—it's medicine. Every night of quality rest directly contributes to faster healing, reduced complications, and a smoother return to normal life. Your future self will thank you for prioritizing sleep during this crucial healing period.
Most importantly, be patient with yourself. Recovery sleep has its own timeline, and improving sleep quality is often a gradual process rather than an immediate transformation. Trust that with the right approach and adequate support, your sleep will return to normal—and may even be better than before your surgery.
Medical Disclaimer
This information is provided for educational purposes only and should not replace professional medical advice. Post-surgical insomnia and recovery sleep needs vary significantly based on the type of surgery, individual health conditions, medications, and personal factors.
Always follow your surgeon's and healthcare team's specific post-operative instructions regarding sleep positioning, activity restrictions, and medication management. These medical guidelines take precedence over any general advice provided in this guide.
Contact your healthcare provider immediately if you experience severe sleep disturbances accompanied by concerning symptoms such as difficulty breathing, severe pain unrelieved by prescribed medications, signs of infection, or significant mood changes that could indicate complications.
If you have persistent insomnia that significantly impacts your recovery or daily functioning, discuss these issues with your medical team rather than attempting to self-treat. Some sleep disturbances may require professional evaluation or specific treatments beyond positioning and environmental modifications.