If you've recently had gastric sleeve surgery and are finding sleep more challenging than expected, you're not alone in this experience.
While gastric sleeve surgery is indeed minimally invasive, the recovery process can bring some unexpected sleep challenges that no one really prepares you for. Your abdomen is healing, and you may be dealing with gas discomfort, tenderness around the incision sites, or simply finding that your usual sleeping positions don't feel quite right anymore. It's common to feel like you're constantly searching for that perfect position where everything feels supported and comfortable.
The good news is that with some thoughtful adjustments to your sleep positioning and environment, you can find comfort again. This phase of recovery is temporary, and there are practical solutions that can help you rest better while your body heals.
Your sleep matters for your recovery, and you deserve to wake up feeling rested rather than like you've been fighting your bed all night. Let's explore some strategies to help you find the comfortable, restorative sleep your healing body needs.
Let's Talk About What's Really Happening
Your body just went through some serious internal renovations. We're talking about a complete stomach reconfiguration project that involved multiple access points (those laparoscopic incisions), internal restructuring (your new sleeve-shaped stomach), and a construction crew that decided to leave behind some CO2 gas as a parting gift.
The result? Your internal architecture is now operating under completely different structural requirements, and your usual sleep positions are about as effective as trying to sleep on a pile of construction materials.
Here's the engineering challenge you're facing:
Your stomach has been resized and repositioned, which means pressure points that never mattered before are now critical structural considerations. The CO2 gas that was used during surgery is currently taking up residence in places it doesn't belong, creating pressure that radiates to your shoulders. Multiple small incisions across your abdomen are in various stages of healing, each requiring protection from pressure and movement. Your digestive system is operating under completely new specifications, where even small amounts of food or liquid can create internal pressure if you're not positioned correctly.
The Position That Changes Everything: Elevated Back Sleeping
Forget everything you've read about "finding comfortable positions." There's really only one position that works consistently during gastric sleeve recovery, and that's elevated back sleeping. This isn't just the "best" option—it's often the only option that addresses all your structural challenges simultaneously.
Think of elevated back sleeping as your recovery headquarters. You're creating a 30-45 degree angle that works with physics instead of against it. This positioning isn't arbitrary—it's engineered specifically to solve the problems your body is currently dealing with.
Why This Position Works When Nothing Else Does
Gas Pressure Management
That mysterious shoulder pain? It's CO2 gas that got trapped in your diaphragm area during surgery. When you're elevated at the right angle, gravity helps move this gas toward areas where your body can actually process and eliminate it. Lying flat keeps the gas exactly where you don't want it.
Internal Pressure Relief
Your newly configured stomach is still figuring out its new job description. Elevation reduces the internal pressure that builds up when you're flat, which directly translates to less nausea and better comfort throughout the night.
Incision Protection
Multiple small incisions means multiple vulnerable spots that can't handle pressure or stretching. Elevated positioning distributes your body weight more evenly, preventing concentrated pressure on any single incision site.
Circulation Enhancement
When you're elevated, your cardiovascular system doesn't have to work as hard to circulate blood effectively. Better circulation means more oxygen and nutrients getting to your healing tissues, which accelerates your recovery timeline.
Mobility Advantage
Getting up from an elevated position requires significantly less core muscle engagement than rising from completely flat. Since your abdominal muscles are currently on modified duty due to surgery, this makes movement much easier and less stressful on your healing incisions.
The 30-45 Degree Sweet Spot
This angle range isn't pulled from thin air—it's the result of understanding how physics works with your healing body. Less than 30 degrees and you don't get adequate gas relief or pressure management. More than 45 degrees and you'll spend all night sliding down your pillow setup, which defeats the entire purpose.
Your progression strategy:
-
Week 1: Start at 40-45 degrees when symptoms are most intense
-
Week 2: Reduce to 35-40 degrees as acute effects improve
-
Week 3+: Settle into 30-35 degrees for sustained comfort

The Sleep Position Hierarchy: What Works and What Definitely Doesn't
Positions That Will Make Your Recovery Miserable
Stomach Sleeping
This is off the table completely. The pressure on your incisions would be like asking fresh wounds to enjoy a wrestling match.
Flat Back Sleeping
While not as obviously problematic, lying completely flat intensifies gas pressure and increases load on your healing stomach structure.
Left Side Sleeping
Your newly configured stomach sits on your left side, making this position particularly problematic during early recovery.
Positions You Might Graduate To (With Time and Approval)
Right Side Sleeping
This might become tolerable sooner than left side sleeping, but only with proper support and your surgeon's clearance.
Supported Side Sleeping
Eventually, you may be able to return to side sleeping with comprehensive pillow support systems, but this requires careful progression.
Your Recovery Headquarters
Elevated Back Sleeping
This is where you'll spend most of your time during the first several weeks. Think of it as your base camp—the position that makes everything else possible.
When Gas Pressure Strikes: Your Emergency Protocols
Gas pressure after gastric sleeve surgery isn't just uncomfortable—it can be genuinely debilitating and often strikes at the worst possible times.
Shoulder Pressure That Makes No Sense
This is the most common complaint, and it confuses everyone because your shoulder wasn't operated on. The culprit is CO2 gas irritating your diaphragm, which creates referred pressure that makes your shoulder feel like it's been overworked and strained.
Your immediate action plan: Temporarily increase your elevation to 50-60 degrees, even if it feels like you're sleeping sitting up. Take gentle walks every 2-3 hours if your surgeon approves—movement helps gas migrate. Apply heat to your shoulder area (never to surgical sites). Stay hydrated with room temperature water. Contact your surgeon if pressure persists beyond the expected timeline.
Abdominal Pressure That Makes Lying Down Impossible
This happens when residual gas and post-surgical swelling create internal pressure that gets worse when you try to lie down.
Your response strategy: Maintain strict elevation for 48-72 hours—don't try to tough it out in flatter positions. Completely avoid carbonated beverages. Use gentle heat on your back or sides, never directly on incisions. Consider temporarily sleeping in a recliner if your bed setup isn't providing adequate relief.
The Equipment Reality: Why Household Pillows Don't Cut It
Here's the uncomfortable truth about trying to create elevation with regular pillows: they're structurally unreliable. Household pillows compress under body weight, shift during normal sleep movement, and lose their positioning exactly when you need support most.
What typically happens with DIY approaches: You spend 20 minutes each night building your pillow foundation, only to wake up at various points when everything has collapsed and you're back to being structurally unsupported. This constant readjustment disrupts your sleep cycles and interferes with the deep sleep your body needs for healing.
The math of DIY pillow solutions:
-
Setup time: 20 minutes nightly
-
Wake-ups for readjustment: 2-4 per night
-
Total cost across multiple pillow purchases: $150-250
-
Success rate: Inconsistent at best

The Best Whole Body Pillow for Gastric Sleeve Surgery Relief
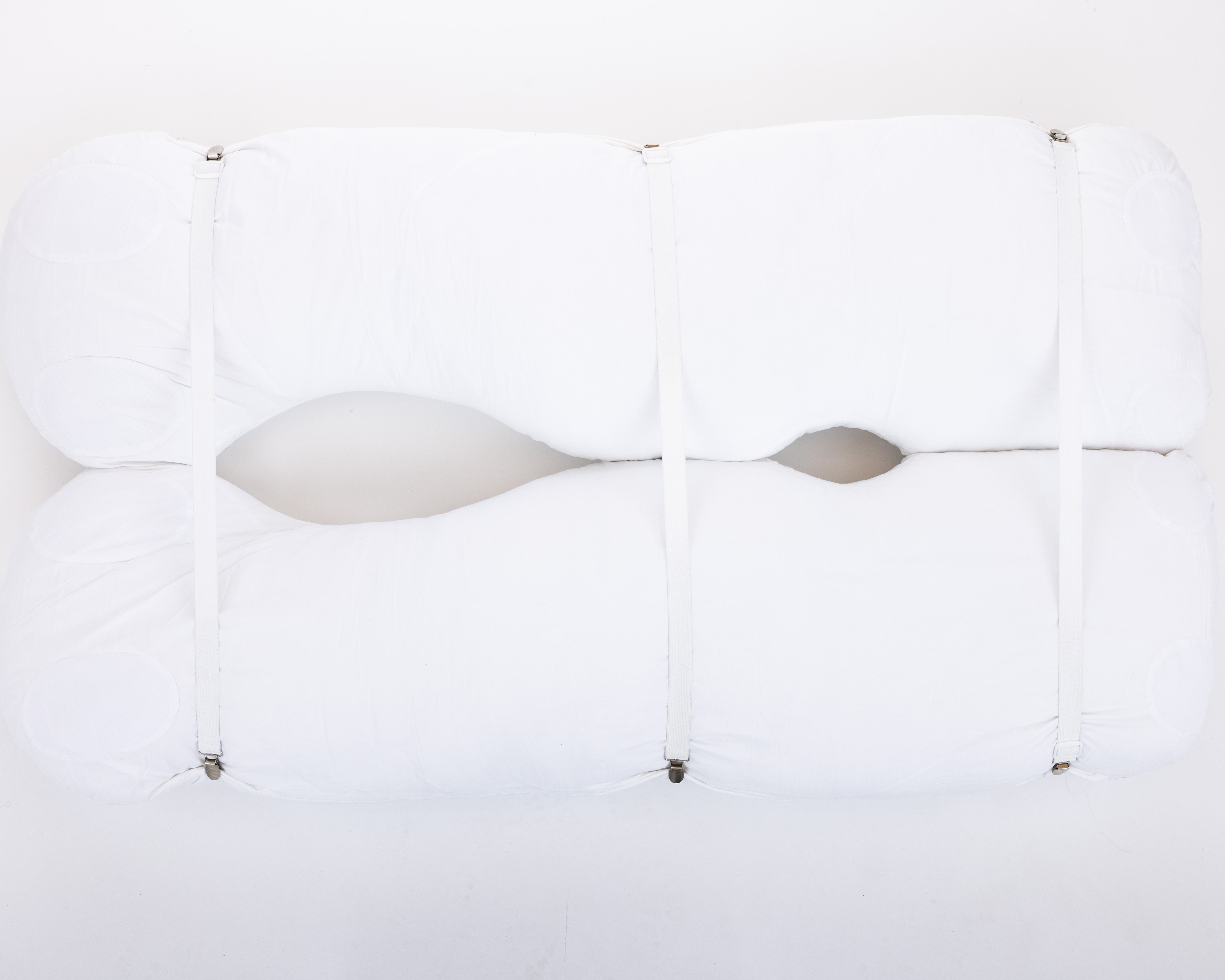
The Sleep Again Pillow System was specifically designed for post-surgical recovery, addressing every positioning challenge we've discussed.
Every Sleep Again Pillow System includes:
-
Two Contoured Side Pillows to cradle back and hips
-
Upper Body Wedge to create optimal upper body incline
-
Leg Support Wedge to gently elevate legs
-
Head Pillow to provide head support and neck mobility
-
Removable, washable slipcovers for every piece
Why this system works better than DIY solutions: The components maintain their structural integrity throughout the night, eliminating middle-of-night collapse situations. Setup takes 3-5 minutes instead of 20. The integrated design ensures all pieces work together rather than fighting each other. Dense foam construction (not memory foam) provides consistent therapeutic angles instead of gradually losing elevation.
Specifically designed for gastric sleeve recovery: The 30-degree wedge angle is optimal for gas pressure relief during recovery. The 30-inch width accommodates full body support without partner displacement. The contoured side pillows prevent unconscious rolling onto healing incision sites. The washable covers maintain hygiene during extended recovery periods when you're spending more time in bed.
HSA/FSA eligible investment: Unlike random pillow purchases, the Sleep Again Pillow System qualifies as a medical expense for most HSA and FSA plans. This positioning system is classified as durable medical equipment, making it a tax-advantaged purchase that supports your recovery.
SHOP THE BEST PILLOW FOR GASTRIC SLEEVE SURGERY RECOVERY
The Emotional Side of Your New Sleep Setup
Let's talk about something most recovery guides completely skip: the emotional adjustment to sleeping with a positioning system. This isn't just about physical comfort—it's about adapting to a completely different relationship with your bed, your sleep space, and even your sense of self during recovery.
It's Normal to Feel Overwhelmed
Your body just went through major surgery, you're learning to eat completely differently, and now your sleep setup looks like mission control. Feeling emotionally resistant to yet another change is completely normal. Many patients describe feeling:
Trapped or Restricted
The elevated position and pillow barriers can initially feel confining, especially if you're used to moving freely during sleep. This sensation of being "held in place" can trigger anxiety about losing control or feeling helpless.
Self-Conscious About the Setup
Your bed now looks like a medical facility rather than your cozy sleep sanctuary. It's normal to feel like the pillows are a visible reminder of your recovery status, making you feel "sick" or "different."
Grieving Your Old Sleep Habits
You might find yourself mourning the simplicity of just falling into bed without thinking about angles, support, and positioning. This grief over lost normalcy is a real part of the recovery process.
Worried About Partner Impact
If you share a bed, you might feel guilty about the space your recovery setup requires or anxious about disrupting your partner's sleep. This can create relationship stress during an already challenging time.
Reframing Your Sleep System as Self-Care
Instead of viewing your positioning system as medical equipment, try thinking of it as your personal healing sanctuary. Many Sleep Again Pillow System users describe their pillow system as their "safe space" or "healing cocoon"—a place where their body can focus entirely on recovery.
Your positioning system represents:
-
A commitment to your healing and long-term health
-
Taking control of your recovery process
-
Prioritizing quality rest that your body desperately needs
-
An investment in faster, more comfortable healing
The Adjustment Timeline
Week 1-2: Resistance Phase
It's normal to feel frustrated with the setup, miss your old sleep positions, and feel emotionally overwhelmed by all the changes in your life. Give yourself permission to feel these emotions without judgment.
Week 3-4: Acceptance Phase
Most patients start to appreciate the consistent comfort and realize they're sleeping better with proper support. The initial emotional resistance begins to fade as physical benefits become clear.
Week 4+: Integration Phase
Many patients find they actually prefer their elevated setup even after recovery. What started as medical necessity often becomes a preferred sleep arrangement that continues providing benefits.
Making Peace with the Process
Communicate with your partner about your needs and feelings. Most partners want to support your recovery and appreciate understanding what you're experiencing emotionally.
Create positive associations with your sleep setup. Use the time in your elevated position for relaxing activities like reading, meditation, or gentle stretching.
Remember the temporary nature of the adjustment period. Your emotional resistance to the positioning system will likely decrease much faster than you expect.
Focus on the healing benefits rather than the inconvenience. Each night of proper positioning is directly supporting your body's recovery and long-term success.
Your Recovery Timeline: What to Expect Week by Week
Week 1: Foundation Phase
Your primary focus is managing gas pressure and protecting incision sites. Elevated back sleeping at 40-45 degrees is non-negotiable. Expect to feel like your internal systems are still figuring out their new configuration. Pain medication timing becomes crucial—take it 30-45 minutes before bedtime to help with positioning comfort.
Week 2: Stabilization Phase
Gas pressure should be significantly improved, but you're still in protection mode. You can reduce elevation to 35-40 degrees if comfortable. Brief experiments with right-side sleeping might be possible, but keep them short (10-15 minutes) and always return to elevated back as your primary position.
Week 3-4: Expansion Phase
You're entering the phase where position variety becomes possible, but elevated back sleeping should remain your home base. Longer periods of side sleeping might be tolerable, but monitor your body's response carefully. Your surgeon may clear you for more position options during this phase.
Week 4+: Adaptation Phase
This is when you start transitioning toward more normal sleep patterns, but the elevation that helped during recovery often continues to provide benefits. Many patients find they prefer sleeping elevated even after full recovery because of improved comfort and digestion.

SHOP THE BEST PILLOW FOR GASTRIC SLEEVE SURGERY RECOVERY
Problem-Solving Common Sleep Challenges
"My pillow setup keeps falling apart during the night."
This is the most common complaint with DIY solutions. The structural integrity of household pillows simply isn't designed for the consistent support needed during recovery. The Sleep Again Pillow System eliminates this frustration completely with dense foam construction that maintains positioning.
"I can't get comfortable no matter what I try."
This usually indicates you're not achieving true elevation or your support system has gaps. The Sleep Again Pillow System's integrated components work together to eliminate gaps and provide comprehensive support.
"My partner can't sleep because of all the pillows"
Recovery positioning does require more space than normal sleep setups. The Sleep Again Pillow System actually uses less bed real estate than most DIY solutions while providing superior support.
"I keep sliding down during the night"
This happens when your elevation surface doesn't have adequate grip or the angle is too steep. The Sleep Again Pillow System is specifically designed to prevent sliding with proper angles and non-slip construction.
The Investment Reality Check
Most patients end up buying 2-3 rounds of different pillows before finding something that works, often spending $150-250 total while dealing with weeks of poor sleep quality.
The hidden costs of inadequate positioning: Extended recovery time requiring additional medical visits. Increased pain medication needs due to poor sleep quality. Higher risk of complications from inadequate rest. Delayed return to normal activities and work.
Professional positioning systems like Sleep Again Pillows: Complete system currently $299.98 (reg. $329.00) for an integrated solution. HSA/FSA eligible purchase means many patients pay significantly less out-of-pocket. Immediate results from night one. Consistent performance throughout recovery and beyond. Quality guarantee with exchange policy for damaged items.
The cost-per-night analysis: At $299.98 for 8 weeks of recovery, that's $5.35 per night for professional-grade positioning that directly supports your healing process. When you factor in HSA/FSA eligibility, the effective cost is often 20-30% lower depending on your tax bracket.
Real cost comparison:
-
DIY pillow approach: $150-250 across multiple purchases + setup time + sleep disruption + no tax benefits
-
Sleep Again Pillow System: $299.98 one-time investment with immediate, consistent results + HSA/FSA eligibility
Why gastric sleeve patients choose Sleep Again Pillows over DIY solutions: The specific 30-45 degree elevation angles required for gas pressure relief. Professional construction that maintains therapeutic positioning throughout 8+ hour sleep periods. Designed by medical professionals who understand post-surgical recovery needs. Eliminates the trial-and-error period when you need reliable positioning most.
Common Questions About Recovery Sleep
How long will I need to sleep elevated after gastric sleeve surgery?
Most patients need elevation for 4-8 weeks, but individual healing varies. Your surgeon will provide specific timelines based on your progress.
Why does my shoulder hurt more than my actual incisions?
This is CO2 gas irritating your diaphragm, causing referred pressure. It's completely normal and should resolve within 1-2 weeks.
Can I damage my new stomach by sleeping in the wrong position?
While you're unlikely to cause permanent damage, poor positioning can increase discomfort and potentially slow healing.
When can I go back to sleeping on my stomach?
Most surgeons recommend waiting 6-12 weeks minimum. Some patients find they need to permanently modify this position.
Should I invest in positioning equipment for temporary recovery?
Quality positioning systems like Sleep Again Pillows often provide immediate results and continue offering benefits long after recovery. The investment frequently pays for itself in improved sleep quality during the crucial early weeks.
When to Contact Your Medical Team
Immediate medical attention required for: Fever over 101°F, severe abdominal pressure that doesn't respond to position changes, signs of infection around incisions, persistent vomiting preventing hydration, or difficulty breathing.
Schedule follow-up discussions for: Sleep problems that worsen after the first week, gas pressure that doesn't improve after 10-14 days, questions about advancing to different positions, or concerns about eating timing and sleep comfort.
Your Sleep Recovery Success Strategy
Gastric sleeve recovery sleep challenges are real, but they're manageable with the right approach. The key is understanding that elevated back sleeping isn't just a suggestion—it's a therapeutic intervention that directly supports your surgical healing and long-term success.
Your recovery blueprint focuses on engineering solutions rather than hoping for comfort. Week 1 prioritizes gas management through strict elevation. Week 2 maintains protection while testing gentle expansion. Weeks 3-4 gradually increase options based on structural healing. Week 4+ transitions to sustainable long-term habits.
Whether you choose a DIY approach or invest in the Sleep Again Pillow System, the goal is creating sustainable comfort that works consistently. Your body is doing incredible healing and metabolic adaptation work, and it deserves optimal conditions for recovery.
Most importantly, understand that recovery isn't linear. Some nights will be better than others, but providing consistent, quality support allows your body to heal effectively while you rest.
Good sleep isn't a luxury during gastric sleeve recovery—it's a medical necessity that directly affects healing speed, metabolic adaptation, and long-term weight loss success. You will sleep normally again. This recovery phase is temporary, even when it feels endless during difficult nights.
Trust the process, listen to your body's structural requirements, and don't hesitate to invest in proper positioning during this crucial healing period.
Medical Disclaimer
This information is provided for educational purposes only and should not replace professional medical advice. Every gastric sleeve procedure and recovery process is unique, and sleeping position recommendations may vary based on your specific surgical approach, individual health conditions, and post-operative circumstances.
Always follow your surgeon's specific post-operative instructions regarding sleep positioning, activity restrictions, and recovery protocols. These medical guidelines take precedence over any general positioning advice provided here.
Contact your healthcare provider immediately if you experience concerning symptoms such as severe abdominal pressure, signs of infection, persistent nausea or vomiting, difficulty breathing, fever, or any symptoms that worsen rather than improve during your recovery period.